A new study points to the responsibility of triclosan, an antibacterial agent very present in our hygiene products, in the resistance of bacteria to antibiotics.

Shower gel, toothpaste, mouthwash, cosmetics and even baby clothes and toys… You may never have heard of it, and yet it’s everywhere: triclosan.
Added by manufacturers to most of our hygiene products, this powerful antibacterial does not only mean good to us. According to a new study conducted by Washington University in St. Louis and published in the journal Antimicrobial Agents & Chemotherapy, it would even contribute greatly to making bacteria resistant to concentrations of antibiotics which should nevertheless be fatal to them. Worse: this antibacterial resistance would also concern infectious agents responsible for common disorders, such as urinary or respiratory tract infections.
Triclosan, a controversial component
First introduced in the 1970s, notably in cleansing gels for surgeons, triclosan is now widely used in beauty and hygiene products, to the chagrin of consumer associations and health authorities.
In 2017, the U.S. Food and Drug Administration cited both safety concerns and lack of efficacy when recommending against adding triclosan to consumer soaps, but these guidelines have not deterred companies. to add it to other products. “In order to effectively kill bacterial cells, triclosan is added in high concentrations to the products,” notes Petra Levin, professor of biology and lead author of the study.
Triclosan reduces the effectiveness of antibiotics by 100 times
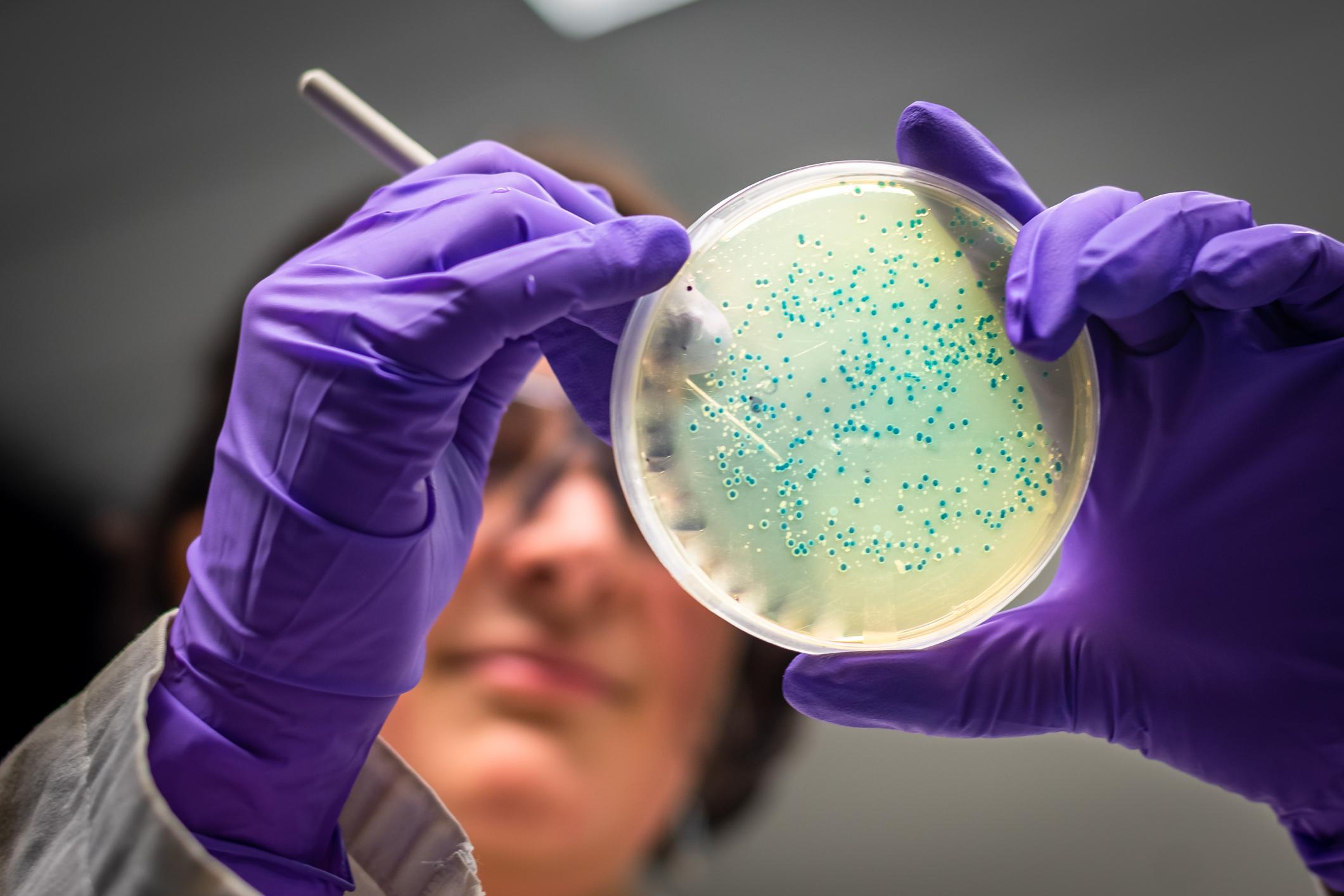
To measure how much triclosan limits the body’s ability to respond to antibiotic treatment, the researchers started by treating bacterial cells exposed to triclosan with bactericidal antibiotics and monitored their ability to survive over time. They then found that triclosan had allowed many bacterial cells to survive.
“Normally, one in a million cells survive antibiotics, and a healthy immune system can control that. But triclosan changed that cell count. Instead of just one in a million surviving bacteria, one in ten organisms survives after 8 p.m. Now the immune system is overwhelmed,” analyzes Petra Levin.
The concern of the researchers lies in particular in the fact that triclosan increases the tolerance of bacteria to a wide range of antibiotics, in particular those treating urinary tract infections. These are common and occur when bacteria, mainly Escherichia coli (E.coli), enter and infect the urinary tract.
By conducting a second experiment on mice with a urinary tract infection, the study authors found that those who drank water enriched with triclosan were not sensitive to antibiotic treatment. “The magnitude of the difference in bacterial load between mice that drank triclosan-treated water and those that did not is striking. We found 100 times more bacteria in the urine of treated mice triclosan, which is a lot”, notes Professor Levin.
Bacteria less susceptible to antibiotics
But how does triclosan interfere with antibiotic treatment? The researchers found that the compound stimulated a small molecule in bacteria dubbed ppGpp (guanosine tetraphosphate), which makes them less sensitive to antibiotics.
In times of stress (when the bacterium is attacked), ppGpp reacts by closing the cell’s biosynthetic pathways, which usually allow it to proliferate. This response allows the bacteria to survive antibiotic attacks, but also to grow stronger.
However, it is precisely by these routes that the antibiotic treatment infiltrates the bacteria to destroy them. When they were exposed to triclosan, the bacteria had already closed the biosynthetic pathways: it was therefore impossible for the bactericidal antibiotic treatment to act effectively.
Clinical studies would be needed to definitively prove that triclosan interferes with antibiotic treatments in humans, says Petra Levin. “I hope this study serves as a wake-up call that helps us rethink the importance of antimicrobials in consumer products.”
.