Microplastics can multiply the number of antibiotic-resistant bacteria up to 30 times once they wash down household drains and enter municipal sewage treatment plants.

- Microplastics in wastewater harbor antibiotic-resistant bacteria and other pathogens, this new study shows.
- Not only shelter for superbugs, these microplastics also participate in their proliferation and increase their antibiotic resistance by forming a biofilm that attracts and retains pathogens.
Microplastics are not only an environmental disaster, helping to devastate marine ecosystems, they are also a health threat. Less than 5 millimeters in size, or 70 times thinner than the diameter of a hair, these microplastics come from our land activities and are found in all our products, from cosmetics to toothpaste and microfibers in clothing, our food, air and drinking water.
Already considered a danger to human health, they could contribute to bacterial antibiotic resistance. In a study published in the Journal of Hazardous Materials Letters, researchers from the New Jersey Institute of Technology (USA) show how, passing through pipes and entering sewage treatment plants, these microplastics can increase the antibiotic resistance of certain bacteria by up to thirty times. strains of bacteria. When they flow through domestic drains and enter sewage treatment plants, these pathogens become trapped in microplastic biofilms that can form inside the pipes.
According to Mengyan Li, author of the study, “These sewage treatment plants can be hotspots where various chemicals, antibiotic-resistant bacteria and pathogens converge”. “What our study shows is that microplastics can act as carriers for these, posing imminent risks to aquatic biota and human health if they bypass the water treatment process.”
3 genes implicated in resistance to common antibiotics
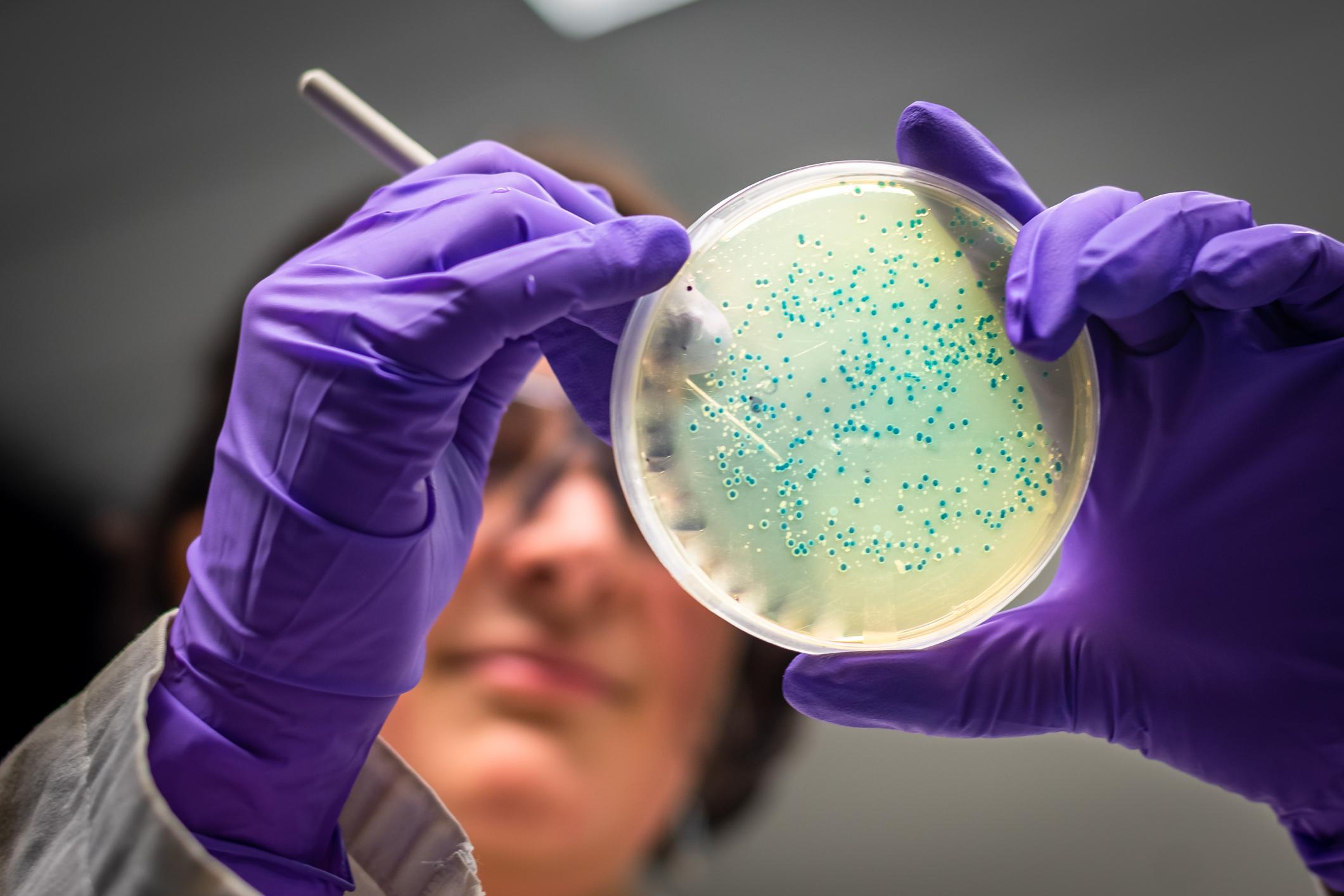
The researchers collected batches of sludge samples from three domestic treatment plants in northern New Jersey. They then inoculated the samples in the lab with two widely used commercial microplastics: polyethylene (PE) and polystyrene (PS). Their goal: to identify the species of bacteria that tend to grow on microplastics, while tracking the genetic changes of the bacteria.
Their analysis revealed that three genes in particular – sul1, sul2 and intI1 – known to promote resistance to common antibiotics, sulfonamides, were up to 30 times more numerous on microplastic biofilms than in laboratory control tests using sand biofilms after only three days.
When the team added an antibiotic, sulfamethoxazole (SMX), to the samples, they found that the antibiotic resistance genes were amplified up to 4.5 times.
This means that it was not just the antibiotics that boosted the resistance genes in these bacteria. Microplastics have also contributed to increasing bacterial antibiotic resistance.
The formation of a glue-like biofilm
Eight different species of bacteria were highly enriched on microplastics. Among them, two emerging human pathogens generally linked to respiratory infections (Raoultella ornithinolytica and Stenotrophomonas maltophilia). Another bacterial strain, Novosphingobium pokkaliiis suspected by scientists to be the key to the formation of the sticky biofilm that attracts and retains pathogens.
“We might think of microplastics as tiny balls, but they provide a huge surface area for microbes to live in, emphasizes Professor Li. When these microplastics enter the sewage treatment plant and mix with the sludge, bacteria like Novosphingobium can accidentally attach to the surface and secrete extracellular glue-like substances. When other bacteria attach to the surface and grow, they can even exchange DNA with each other. This is how antibiotic resistance genes spread through the community.”
.