Antibodies to fight HIV. An American team has developed immunotherapy that suppresses the viral load in humans, including in reservoir cells.

- Antiretroviral therapy does not attack HIV reservoirs
- Immunotherapy was abandoned because of its effectiveness
- New antibody therapy suppresses viral load, including in HIV host cells
Aids research lights up with a ray of hope. Immunotherapy treatment has been shown to be effective against HIV. It reduced the viral load, including in the reservoirs of the virus. The results of this phase I trial are published in the prestigious journal Nature.
Effective against 80% of strains
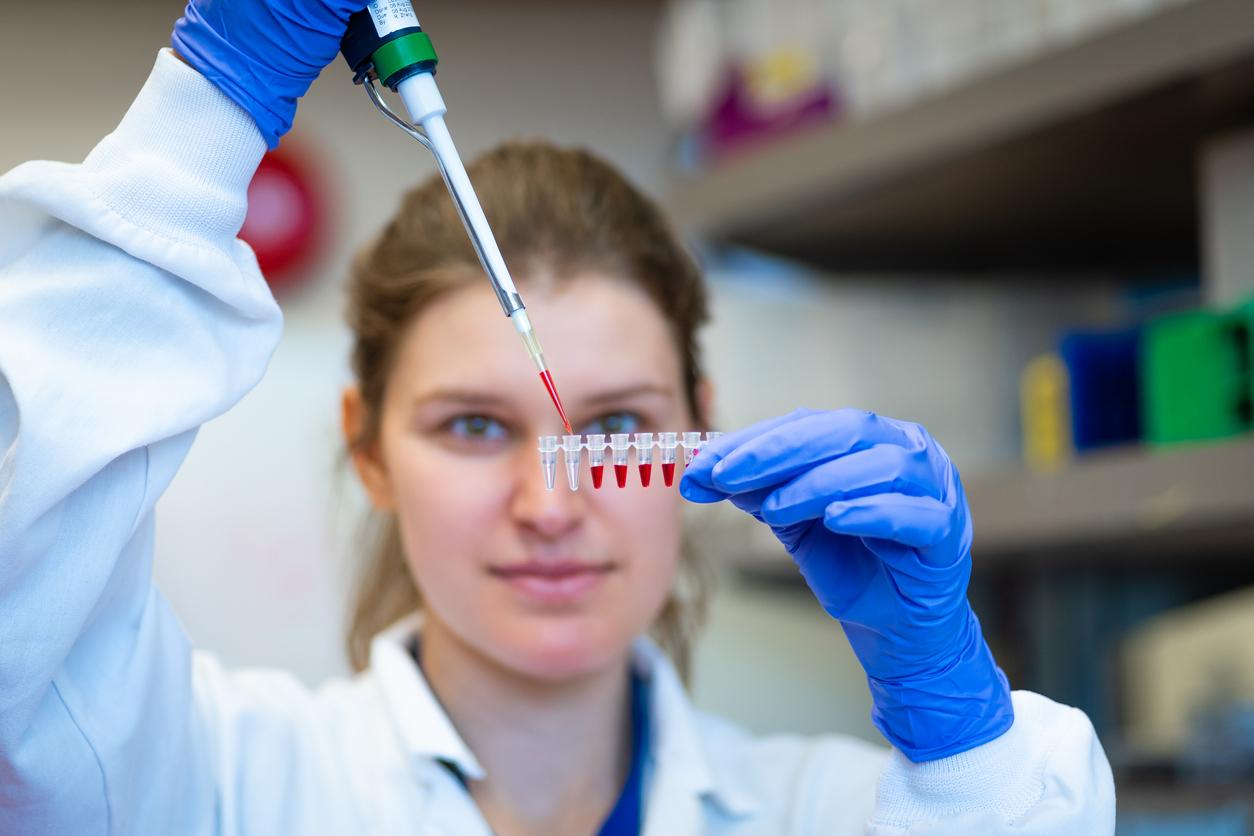
29 volunteers, including 17 HIV carriers, tested innovative immunotherapy. It belongs to a new generation of broad spectrum neutralizing antibodies. They are produced only by a minority of HIV-positive patients (10 to 30%), and only after several years of infection. At this stage, the virus has evolved enough to escape the strongest antibodies. Administering them early would therefore be a solution.
A team from Rockefeller University (New York, United States) isolated and cloned specific broad spectrum neutralizing antibodies: 3BNC117. They target CD4 + T cell binding sites on the HIV envelope, and CD4 receptors at the site of the virus attachment to host cells. “What’s special about these antibodies is that they have activity against 80% of HIV strains, and they are extremely potent,” said Marina Caskey, co-author of the study. They have therefore been transformed into therapeutic agents against the virus. Study participants received different doses intravenously: 1, 3, 10, or 30 milligrams.
Towards a vaccine?
3BNC117-based immunotherapy is well tolerated and safe in humans. The higher dosages caused the viral load to drop sharply and rapidly, even after 8 weeks. More importantly, the antibodies attacked viruses “hidden” in infected cells, which antiretroviral therapy cannot. The resistance of HIV to this new treatment is variable. “Unlike conventional antiretroviral therapy, antibody therapy can also stress the patient’s immune cells, which can help neutralize the virus better,” adds Florian Klein, co-author of the study.
Another benefit, and not the least, is that such treatment should only be administered occasionally. It should, however, be used in combination with other therapies. “An antibody alone, just like a drug alone, is not enough to suppress the viral load in the long term, because resistance will set in,” recalls Marina Caskey, however.
This phase I clinical trial therefore demonstrates the feasibility of antibody-based immunotherapy, a technique abandoned because it is ineffective. There is hope, as the 3BNC117 antibodies speed up HIV, preventing it from mutating to defend itself as it usually does. In the laboratory, on animal models and in humans, the results remain excellent. So much so that researchers do not rule out the development of a vaccine that blocks the infection even before it sets in.
.