In France, the coronavirus (covid-19) would have contaminated less than 5% of the population, far from collective immunity, estimate the researchers in epidemiology of the Pasteur Institute on May 13. Even in the regions most affected by the coronavirus (Ile-de-France and Grand Est), less than 10% of the inhabitants were contaminated, according to this study published in Science. These estimates, which are based on models and hospitalization and health data, should nevertheless be taken with caution.
A study conducted by the Institut Pasteur this time using real data on the first cluster of coronaviruses in France, the municipality of Crépy-en-Valois, shows that 25.9% of teachers, high school students and their families have been infected with the disease and have developed antibodies against the virus. What’s more, only 17% of the parents of the high school students concerned, and 21% of their brothers and sisters, were infected with Covid-19. The researchers conclude that the risk of family contamination was relatively low, for people living under the same roof, at a time when we did not know that the coronavirus was circulating and therefore without special precautions, which does not bode well for have collective immunity.
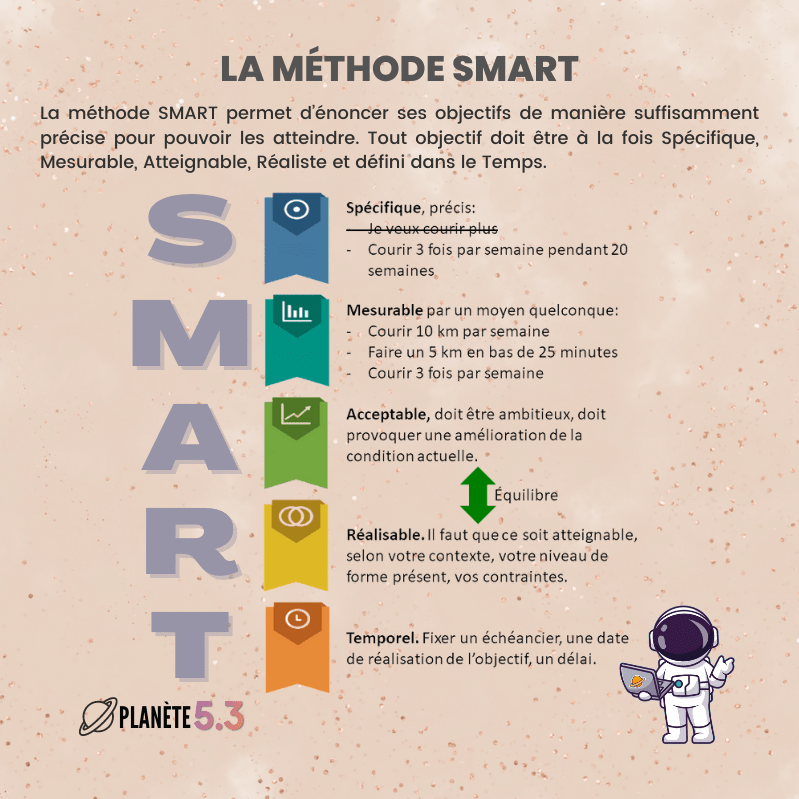
Collective immunity: definition. We speak of “collective immunity” when, in a given population, a pathogen (a virus, a bacterium, etc.) can no longer spread because a majority of people are resistant to it.
“This does not mean that the pathology has disappeared: it can still affect the most fragile people (the elderly, people suffering from chronic or immunocompromised diseases, etc.) but it is no longer spreading in the population – the risk of an epidemic is so very low“explains Pr. Michel Cogné, doctor and professor of immunology.
An example to understand. When a fire breaks out in a forest, the trees near the source of the fire burn and then the flames spread among the trees: in the end, the whole forest goes up in smoke. On the other hand, if a majority of trees are fireproof (that is to say: they have been made fire resistant by various means), only the trees which are at the center of the fire are destroyed: the fire cannot spread and the forest is safe.
“It is not necessary that the whole population is resistant to the virus / to the bacteria: it is enough that the majority of the individuals is it to make “barrier” to the infection.“specifies Pr. Cogné.
How to achieve collective immunity?
“Faced with a pathogen, schematically, we can say that a population is made up of fragile individuals and non-fragile individuals, explains Pr. Cogné. If non-frail individuals are infected with the pathogen, they will develop the disease very mildly (or even asymptomatically) but will mostly acquire antibody specific. Thus, each time they are in contact with the pathogen again, it will be immediately recognized by the antibodies and destroyed: individuals will therefore not be able to transmit the pathology.. “
To achieve collective immunity, it is therefore necessary both to protect the most fragile individuals (for example: thanks to containment measures) while exposing non-fragile populations to the maximum extent to the pathogen (for example: by leaving schools open and active businesses).
“However, there is still a risk for these so-called “non-fragile” populations because complications from the infection are still possible – even if they are rarer. This strategy prevails in France for common infections such as varicella, where the majority of people are allowed to develop the disease and where the vaccine is only offered to the most fragile children!“
The n ° 1 tool to safely achieve collective immunity is the vaccination : “this leads to the production of antibodies specific to a pathogen without the need to contract the disease and risk the hazards thereof: the vaccinated individuals become resistant to the disease and thereby participate in the immunity of the population up to collective immunity“affirms Pr. Cogné.
This was how smallpox, an infectious disease for which a vaccine was discovered at the end of the 18th century, was defeated. “Vaccination of the majority of the population made it possible to prevent the spread of the disease: it gradually disappeared – this is an example of total victory, of collective immunity against a pathogen.“
Second tool in favor of collective immunity: the barrier gestures and in particular social distancing. “If we take the image of the forest fire, failing to protect the trees against the fire, we can already move them away from each other: this makes the spread of the fire more difficult, even if it does not. not stop completely.“
How do you know that you have achieved collective immunity? “It is an observation datum. We cannot really measure collective immunity: it is considered to be reached when the epidemic stops since the pathogen can no longer spread “explains Pr. Cogné.
Collective immunity and coronavirus: where are we?
Covid-19 (the disease caused by the Sars-Cov-2 viral infection) is very contagious: experts estimate that on average, an infected person is able to transmit the Sars-Cov-2 coronavirus to 2 or 3 other individuals. The disease “R0” is said to be 2-3.
“However, this is only an average: the R0 is probably higher in places of community life (for example: on the aircraft carrier Charles-de-Gaulle) or in countries where physical contact is cultural ( thus, it is undoubtedly more important in Spain than in Japan)“adds the specialist.
“To achieve collective immunity against Sars-Cov-2 coronavirus, 60% of the population should have been infected and developed specific antibodies“affirms Pr. Cogné. However, according to a projection carried out by researchers at the Institut Pasteur, as of May 11, 2020, less than 6% of the French population will have been exposed to the Sars-CoV-2 coronavirus. In certain regions ( like the Grand Est), this rate may rise to 12%: this remains insufficient to achieve collective immunity!
And abroad ? “Sweden has bet on collective immunity by recommending that fragile people stay confined to their homes while maintaining the activities (schools, businesses, etc.) of non-fragile people in the face of the Sars-Cov-2 coronavirus“, explains Pr. Cogné. However, at present and according to official statistics, less than 1% of Swedes have contracted the virus …
Is herd immunity an effective strategy against the coronavirus?
It is still too early to tell. “The problem is, very little is known about this Sars-Cov-2 coronavirus“underlines Pr. Michel Cogné.
Main uncertainty: do antibodies produced following infection with the Sars-Cov-2 coronavirus provide temporary or permanent resistance to the virus?
“When you catch a common cold, our body produces antibodies that protect us against new infection for only a few months; in contrast, it has been found that people who have been infected with SARS coronavirus in 2003 today have antibodies that are still effective against this disease: how do you know to which category the Sars-Cov-2 coronavirus belongs?“
There is, moreover, a major difficulty: the figures which reflect the spread of the coronavirus in the world population are not necessarily 100% reliable … “On the one hand, some countries where the epidemic is rife are not democratic, which gives figures that are sometimes far from reality; on the other hand, we know that the coronavirus screening tests are only effective in 68% of cases.“
Conclusion? “The strategy of collective immunity (the one that has been displayed by Sweden or Iran) is a bet, concludes the specialist. We will not know if this was a “good strategy” for a few months, seeing how the infection is maintained or is extinguished in different parts of the world. “
“Some countries which have not (or little) confined will undoubtedly achieve collective immunity naturally … but paying a heavy price in terms of victims of the disease. In view of the frequency of complications, it would be much wiser to count on a coronavirus vaccination to enable us to achieve collective immunity.“
Thanks to Prof. Michel Cogné, doctor and professor of immunology at the Limoges medical school, former member of the scientific council of the Foundation for Medical Research (FRM).
Read also :
Can the coronavirus reach our brains?
Will the coronavirus be recognized as an occupational disease?
Coronavirus: how can one person infect an entire supermarket?