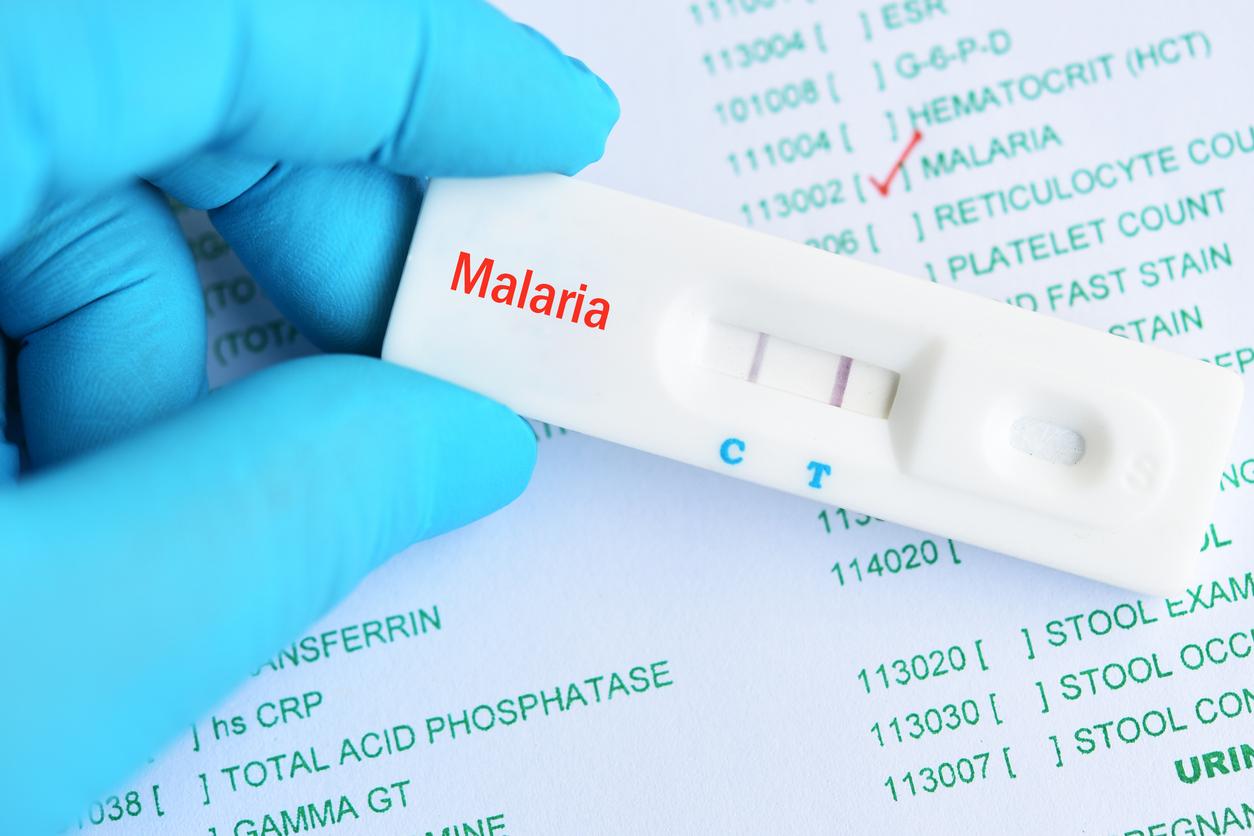
Papillomavirus (HPV) infection is responsible for around 3,000 new cases of Cervical cancer, 500 cancers of the vulva, 300 cancers of the vagina and 1100 cancers of the anus. HPV vaccines have been available for more than 10 years and for cervical cancer, screening every 3 years by smear is recommended.
“In 90% of cases, cervical cancer is due to a persistent infection caused by one or more human papillomavirus (HPV), which is transmitted sexually. There are vaccines, but the population is insufficiently vaccinated. And some of the women are not screened regularly enough “ underlines the HAS.
It is in this context that the Haute Autorité de santé evaluated a new HPV vaccine (Gardasil 9) in order to shed light on the merits of its reimbursement and on the setting of its price.
One of the lowest vaccination rates in Europe
The vaccine coverage rate against the human papillomavirus is one of the lowest in Europe: less than 20% of the target population is vaccinated while the Cancer Plan 2014-2019 sets a target of 60%. “Regarding the screening of Cervical cancer, we know that to date nearly one in two women is not screened regularly enough, which is why a screening organization will be implemented by the National Cancer Institute (INCa) in 2018 “ insists HAS.
Read also : Boys should also get the HPV vaccine
Currently, two vaccines are available and reimbursed as part of the HPV vaccination: Cervarix and Gardasil. The Gardasil 9 vaccine, currently evaluated by the HAS, protects against 5 additional genotypes, thus giving it protection against 90% of cervical cancers linked to HPV. HAS “recognizes its high efficacy and good tolerance, close to that of Gardasil. It therefore offers it for reimbursement by assigning it an important medical benefit”. On the other hand, a price higher than that of Gardasil does not seem justified.
The High health authority recommends also the development of interventions facilitating vaccination, in particular among the least advantaged populations in which recourse to vaccination and screening is less frequent.
Read also :
Cervical cancer: a risk even after 65 years
Cancers: they will increase faster in women in 20 years