Thanks to new brain imaging techniques, researchers have succeeded in predicting the evolution of neurodegeneration in patients suffering from Alzheimer’s. Ultimately, these discoveries could lead to personalized treatments.

Alzheimer’s disease is the leading cause of dementia worldwide. According to the WHO, 50 million people are now affected and, due to the aging of the population, these figures are not about to improve. But today, scientists from the Center for Memory and Aging at the University of San Francisco (UCSF, USA) made great strides in this area. Thanks to new brain imaging techniques, they succeeded in predicting the evolution of the disappearance of neurons from the cerebral cortex during the disease. The results of this study were published on 1er January in the magazine Science Translational Medicine. Ultimately, their discoveries could help refine the prognosis of patients and personalize their treatment.
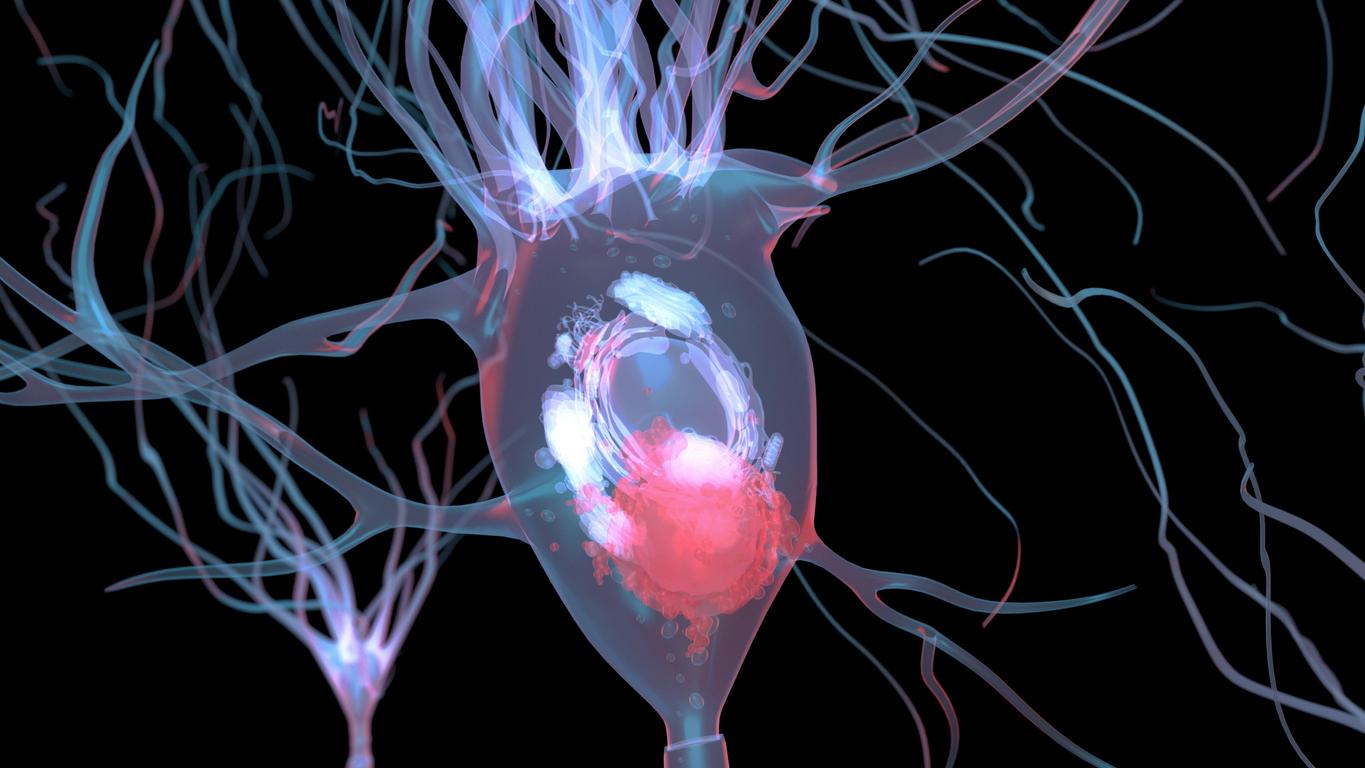
Alzheimer’s is characterized by amyloid protein deposits that form plaques between neurons first and then tau protein deposits inside neurons. For years, researchers have focused on the importance of amyloid plaques and developed drugs that target this aspect of the disease. Today, more and more scientists are interested in tau, which they believe could be an important biological marker of the disease.
“Nobody doubts that amyloid plays a role in Alzheimer’s disease, but more and more discoveries about tau are starting to change the way people think about what is really driving the disease, explains the Professor Renaud La Joie, lead author of the new study. Yet just by examining postmortem brain tissue, it has been difficult to prove that tau tangles cause brain degeneration and not the other way around. One of the main goals of our group has been to develop non-invasive brain imaging tools that would allow us to see if the location of tau accumulation early in the disease predicts later brain degeneration.”
“Tau is a key factor in neurodegeneration”
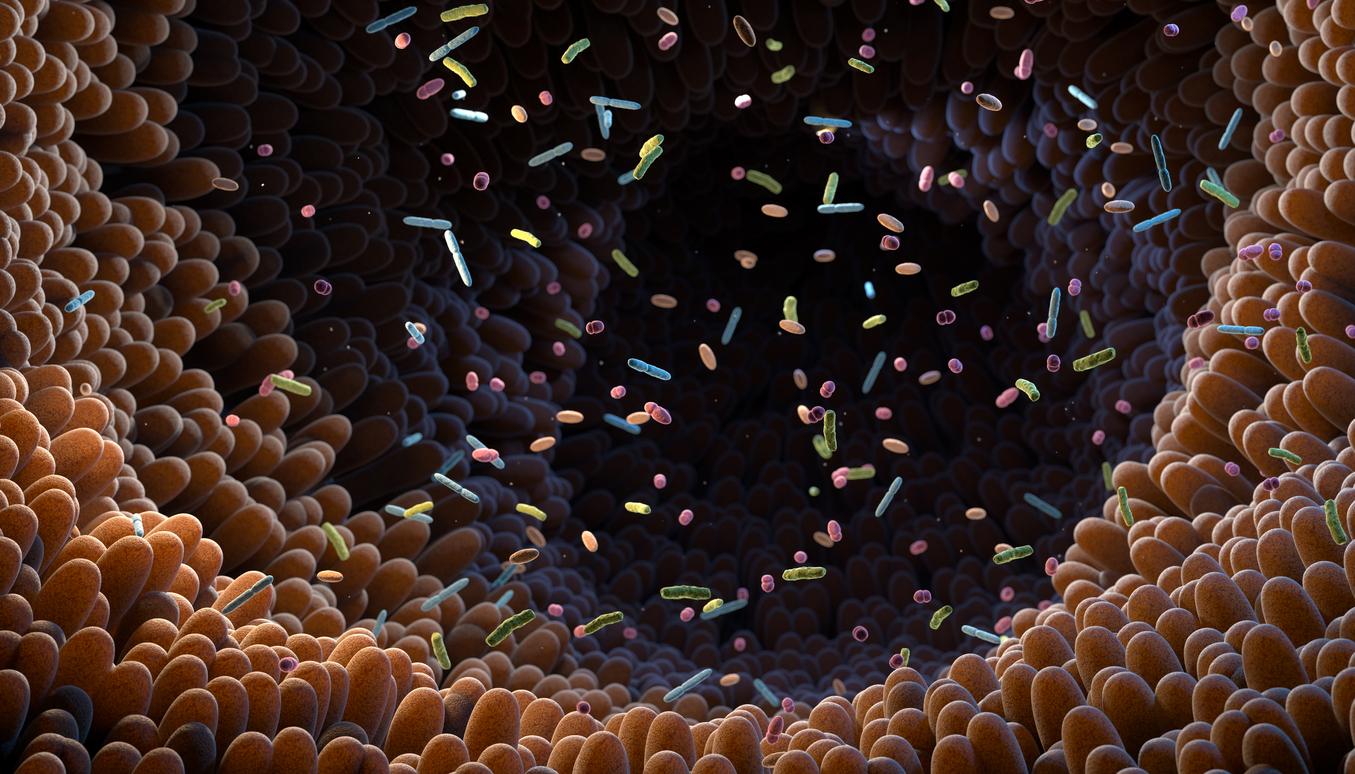
In their study, Renaud La Joie and colleagues recruited 32 participants with early clinical Alzheimer’s disease and had them undergo positron emission tomography (PET) using two different tracers to measure levels of amyloid protein and tau protein in their brains. Participants also had MRI scans to measure the structural integrity of their brains at the start of the study and at follow-up visits one to two years later.
The researchers then realized that the overall levels of tau protein in the participants’ brains at the start of the study predicted the extent of degeneration 15 months later. What’s more, the tau accumulation models predicted atrophy in the same places with more than 40% accuracy.
“Seeing that tau accumulation predicts where degeneration will occur supports our hypothesis that tau is a key factor in neurodegeneration in Alzheimer’s disease,” explains Renaud La Joie.
Very powerful predictions
PET scans also revealed that younger study participants had higher overall levels of tau in the brain and a stronger link between baseline tau and subsequent brain atrophy. Thus, other factors, such as other abnormal proteins or vascular lesions, could play a role in the late onset of Alzheimer’s.
“The correspondence between the spread of tau and what happened to the brain the following year was really striking,” says neurologist Gil Rabinovici, head of the PET imaging program at UCSF’s Memory and Aging Center. “PET Tau imaging predicted not only how much atrophy we would see, but also where it would occur. These predictions were much more powerful than anything we’ve been able to make with other imaging tools, and add to the evidence that tau is an important factor in disease,” he continues.
These discoveries could therefore make it possible to develop more effective drugs and to further personalize the care of people with dementia. This is currently impossible due to the great variability of the disease from one patient to another.
“Giving patients an idea of what to expect”
“One of the first things people want to know when they hear a diagnosis of Alzheimer’s disease is simply what the future holds for them or their loved ones. Will it be a long memory wipe or a rapid decline into insanity? How long will the patient be able to live independently? Will he lose the ability to speak or move on his own? These are questions that we cannot currently answer, except in very general terms, continues Gil Rabinovici. Now, for the first time, this tool could allow us to give patients an idea of what to expect by revealing the biological process underlying their disease.”
More than 200,000 new cases of dementia diagnosed each year in France
“Tau PET could be an extremely valuable precision medicine tool for future clinical trials (…) The ability to sensitively track tau accumulation in living patients would for the first time allow clinical researchers to find treatments that can slow or even prevent the specific trajectory of brain atrophy predicted for each patient,” he concludes.
In France, more than 1,175,000 people suffer from Alzheimer’s disease. The disease is most often manifested by memory problems, then other brain functions are affected. Gradually, the daily tasks are more and more difficult and adapting to new situations becomes almost impossible for the patients. Each year, more than 200,000 new cases of Alzheimer’s or another form of dementia are diagnosed.

.