The new wearable sensors can monitor levels of metabolites and nutrients in a person’s blood by analyzing their body sweat.
-1576144612.jpg)
You don’t like having blood tests when you go to the doctor? Although this banal examination is insurmountable for needle phobics or those who pass out at the sight of blood, the result of a blood test remains a very good indicator of our state of health. However, a new, less invasive technique will soon emerge.
A group of researchers at the California Institute of Technology, led by Wei Gao, assistant professor of medical engineering, have designed a wearable, mass-manufacturable sensor that can monitor levels of metabolites and nutrients in the blood of a person just by analyzing their sweat. This new sensor is more sensitive than those available on the market. Previously developed products mainly targeted compounds in high concentrations, such as electrolytes, glucose and lactate. All results were presented in the review Nature Biotechnology.
The development of this new sensor will allow doctors to continuously monitor the condition of their patients, especially those suffering from cardiovascular diseases, diabetes or kidney problems which can lead to abnormal levels of nutrients or metabolites in the blood. . This process will prevent patients from using an invasive and painful method to monitor their state of health, as is the case with the hypodermic needle, for example. “Such wearable sweat sensors have the potential to quickly, continuously and non-invasively capture health changes at the molecular level,” says Wei Gao. They could allow personalized follow-up, early diagnosis and rapid intervention.”
Using Microfluids for Best Results
Wei Gao’s wearable device uses microfluids to obtain his information. Microfluids are ideal because they minimize the influence of sweat evaporation and skin contamination on detection accuracy. Additionally, as the supplied sweat flows through the microchannels, the device can accurately measure and sense changes in concentrations.
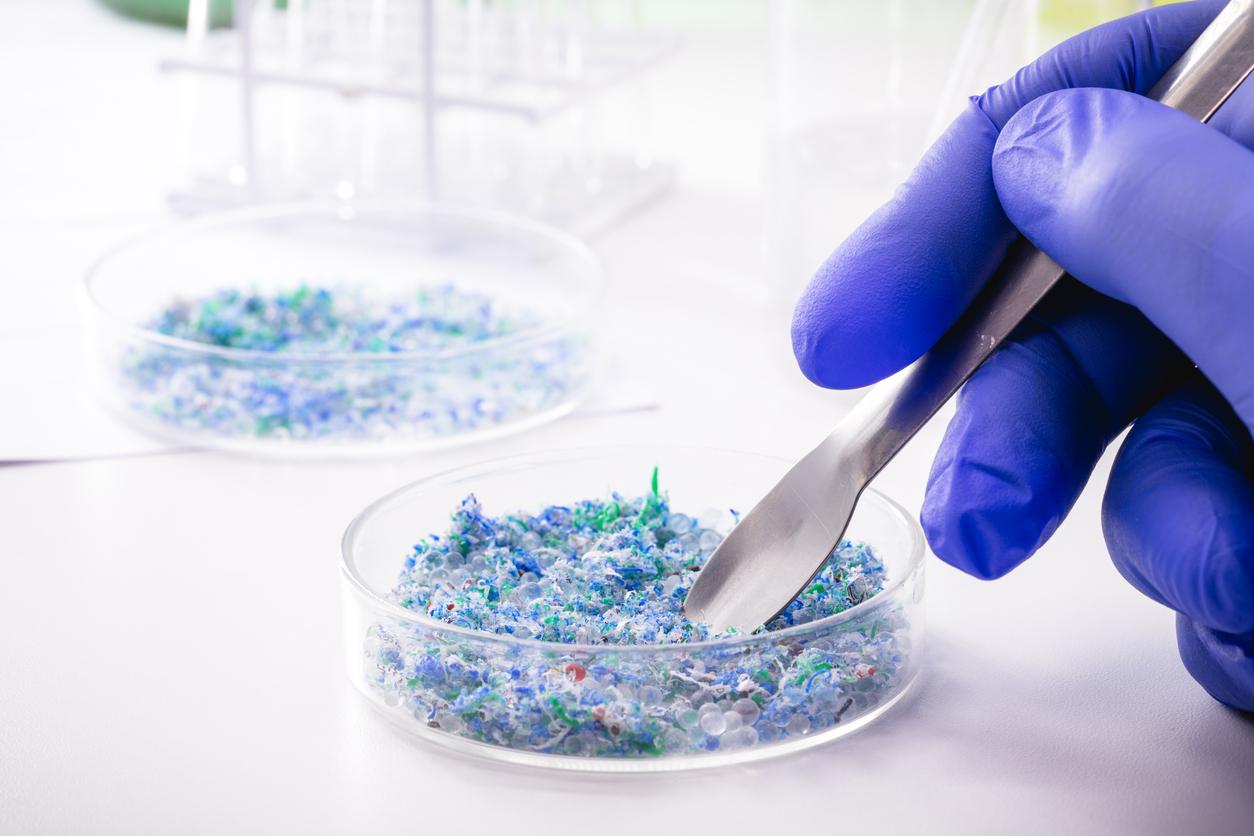
Until now, wearable sensors based on microfluids were fabricated with a lithographic-evaporation process, which requires complicated and expensive fabrication processes. For its sensors, the research team chose to measure respiratory rate, heart rate, and uric acid and tyrosine levels through its sensor.
According to the researchers, the choice of tyrosine is a good one, as it is an indicator of metabolic disorders, liver disease, eating disorders and neuropsychiatric disorders. Uric acid, on the other hand, was chosen because high levels are associated with gout, a painful joint condition that’s on the rise worldwide. Gout occurs when high levels of uric acid in the body begin to crystallize in the joints, especially those in the feet, causing irritation and inflammation.
Device Operation
The researchers conducted a series of tests with healthy patients to find out if the device worked properly. The researchers compared the results of trained athletes and people of average physical condition to check tyrosine levels in sweat, which are influenced by a person’s physical condition. The sensors showed lower levels of tyrosine in the athletes’ sweat. Similarly, to check uric acid levels, researchers monitored the sweat of healthy people both on an empty stomach and after a meal high in purines, food compounds that are metabolized into uric acid. The sensor showed that uric acid levels increased after the meal. To ensure the accuracy of the reading, Wei Gao’s team also performed a similar test on gout patients. The patients’ uric acid levels were much higher than those of healthy people, according to sensor data.
To further verify the accuracy of the sensors, Wei Gao and his colleagues cross-checked the accuracy of the sensors with the tests of blood samples from gout patients and healthy subjects. The results of the sensor are identical to those of the blood sample.
“As nutrients and metabolites are linked to a number of health issues, the information gathered using these wearable sensors will be invaluable for both research and medical treatment,” concludes Wei Gao.
.