Increased exposure to PFAS is associated with kidney damage which could be explained by the action of these eternal pollutants on the intestinal flora.
- A proof-of-concept study in 78 people shows that increased exposure to PFAS leads to decreased kidney function four years later.
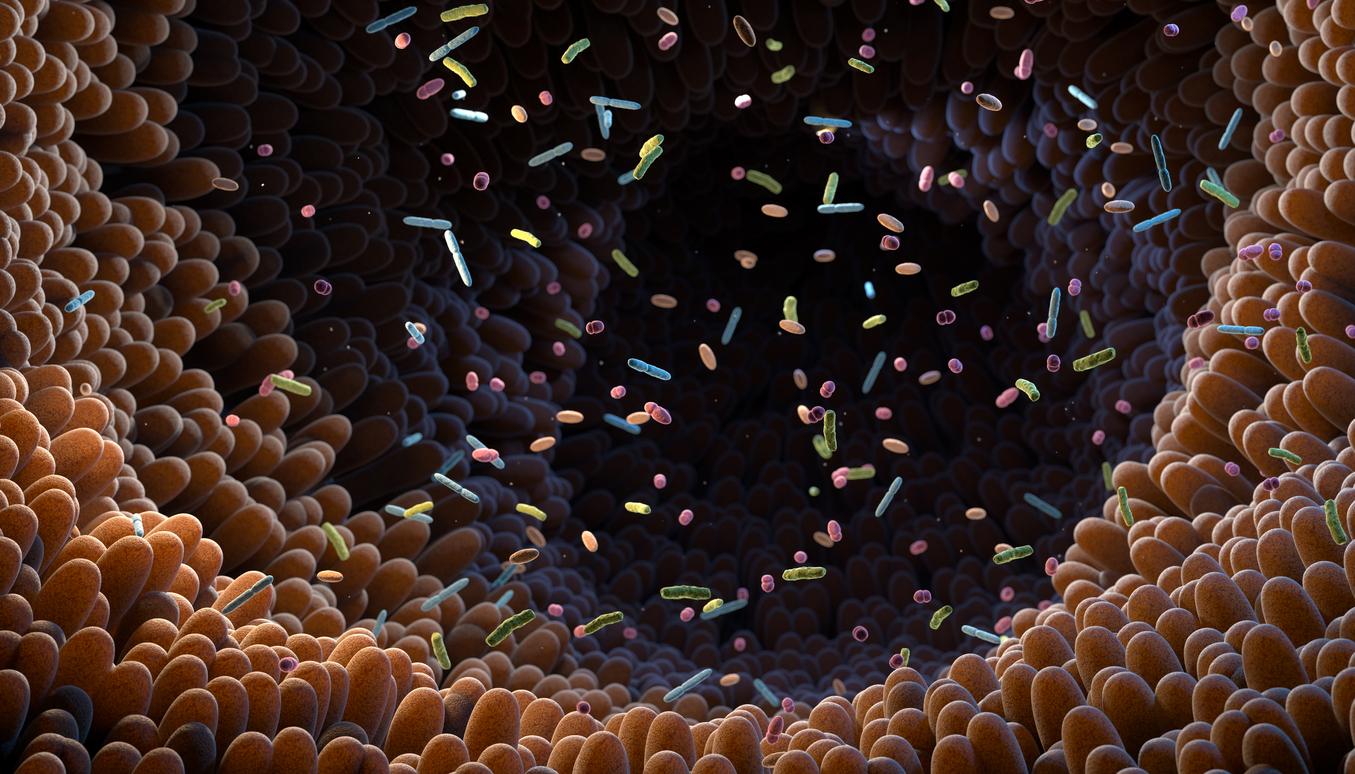
- The work also shows that exposure to PFAS potentially alters microbiome composition, associated with lower levels of beneficial bacteria and lower anti-inflammatory metabolites.
- “This indicates that inflammation and oxidative stress are potential mechanisms [pour expliquer la diminution de la fonction rénale, NDLR]so this is an area on which future research can focus,” says one of the lead authors of the study.
PFAS, per- and polyfluoroalkyl substances, are known to increase the risks of many health disorders such as cancers, cardiovascular diseases and chronic kidney diseases. But the biological mechanisms behind all this are still poorly understood. “Almost everyone has PFAS in their blood, and these chemicals are associated with a number of negative health effects”, confirms Dr. Hailey Hampsonpostdoctoral researcher in population and public health sciences at the Keck School of Medicine of USC. “But we don’t know of any interventions to reduce PFAS in the body, so we can’t really provide recommendations to help.”
In a proof-of-concept study, Dr. Hampson and her colleagues at the Keck School of Medicine of USC looked specifically at the link between PFAS and kidney damage. Their work, published in the journal Science of the Total Environmentshow that increased exposure to PFAS is associated with kidney failure four years later, and that changes in the gut microbiome and associated metabolites could explain up to 50% of the decline in kidney function. “This study raises the possibility of future targeted interventions that can alter the gut microbiome or circulating metabolite profiles to prevent PFAS-induced kidney injury”, indicate the authors.
As exposure to PFAS increases, kidney function declines
To conduct this research, data from 78 participants, aged 17 to 22, enrolled in the Southern California Children’s Health Study – a large-scale longitudinal study aimed at understanding the effects of pollution on health – were analyzed. 56% of the sample was Hispanic because this is a group that is at increased risk for chronic kidney disease.
To measure participants’ exposure to PFAS, gut microbiome bacteria, and circulating metabolites, researchers took blood and stool samples at the start of the study and four years later. They found that each standard deviation increase in the baseline PFAS load score led to a 2.4% drop in kidney function. Next, the group of scientists performed a statistical analysis to determine whether a third factor, gut bacteria and associated metabolites, could contribute to this association.
Exposure to PFAS can alter the composition of the gut microbiota
“We found that PFAS exposure potentially altered microbiome composition, associated with lower levels of beneficial bacteria and lower anti-inflammatory metabolites”, explains Dr. Hampson. In detail, the analysis revealed that a joint component (characterized by a reduction of Lachnospiraceae and 17b-estradiol and an increase of succinate, retinoate and dodecanoic acid) and a metabolite component (characterized by an increase of hypotaurine and a reduction in D-pinitol and ureidopropionate) mediated respectively 38% and 50% of the effect between the PFAS load score and the glomerular filtration rate (a value which makes it possible to quantify the activity of the kidney). “This indicates that inflammation and oxidative stress are potential mechanisms [pour expliquer la diminution de la fonction rénale, NDLR]so this is an area that future research can focus on”, adds the specialist, satisfied with having a road map to continue her studies.
“Our findings provide an important piece of the puzzle regarding the many different health risks of PFAS, which can provide policymakers with information that helps them develop policies to protect the public from exposure to these chemicals”, concluded Dr. Jesse A. Goodrich, assistant professor of population and public health sciences at the Keck School of Medicine and second lead author of the study.