180,000 Dutch people have it, sometimes without knowing it
Tiredness, shortness of breath, tickling cough and poor sleep: maybe it’s heart failure. Fortunately, doctors are increasingly able to detect heart failure at an early stage. The most frequently asked questions:
1 What is heart failure?
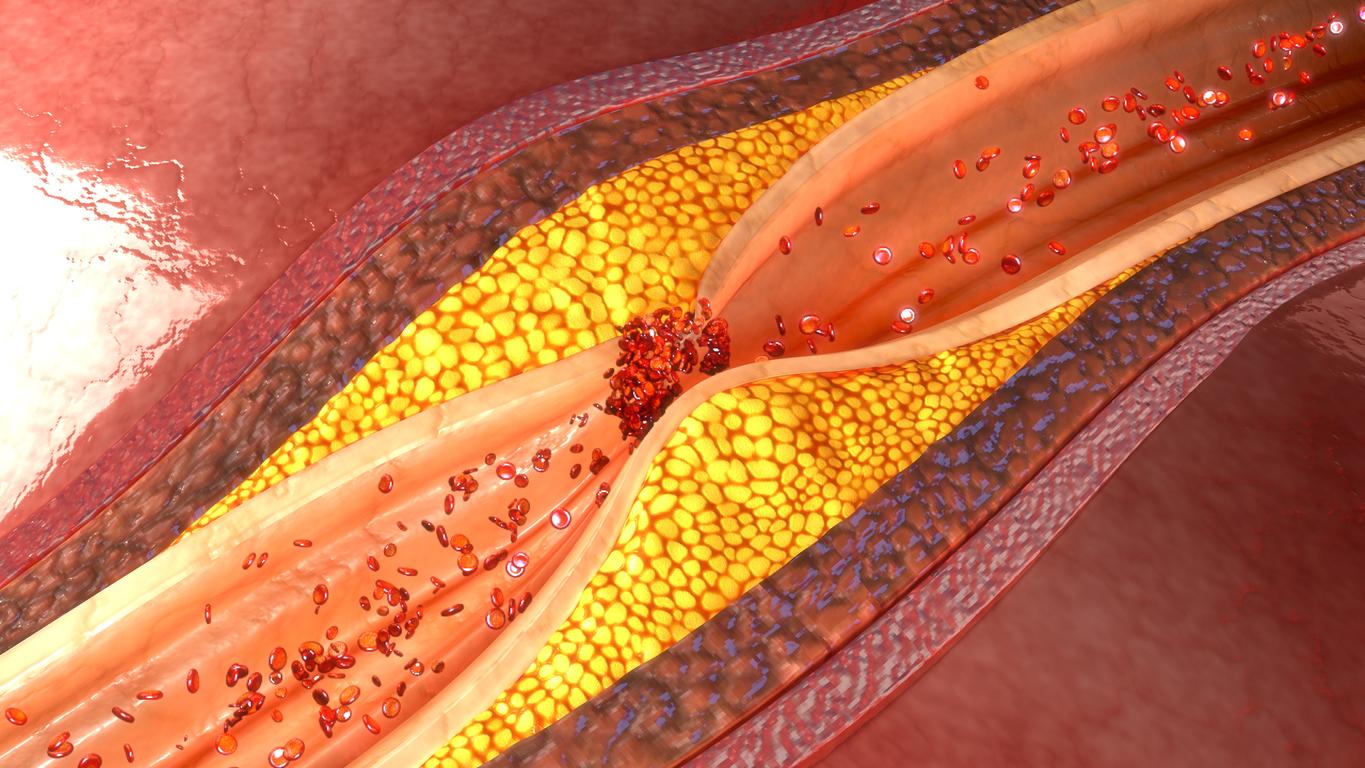
Contrary to popular belief, heart failure is not a disease, but a collective name for symptoms and complaints. These occur when the heart muscle is no longer able to pump blood through the body due to damage. Any condition that damages the heart can lead to heart failure. In about 80 percent of cases, a heart attack is the culprit. Other possible causes are long-term high blood pressure, an infectious disease in the heart muscle (cardiomyopathy) or malfunctioning heart valves.
Broken heart muscle cells do not recover. Instead, stiff connective tissue forms. The stiffer the heart muscle, the harder the heart fills with blood.
When we talk about heart failure, we usually mean chronic heart failure. This means that the symptoms develop gradually. There is also acute heart failure; the heart then suddenly stops functioning, for example due to an inflammation of the heart valve. This article is about chronic heart failure.
2 What do you notice about heart failure?
If the pumping function of the heart stops working properly, blood will accumulate in front of the heart, or the heart will not pump out enough blood. As a result, all kinds of complaints arise. Depending on the severity of the heart failure, these only occur during (strenuous) exertion or at rest.
The body may begin to retain fluid, causing the patient to gain weight in legs and ankles and gain weight without additional food. As the blood accumulates in front of the heart, the pressure in the pulmonary blood vessels rises. This makes the lungs stiffer and less mobile. This results in shortness of breath and a tickly cough, especially with exertion. The cough and shortness of breath get worse when you lie down. Furthermore, heart failure patients have to urinate more often and especially more at night than during the day.
Research shows that 66 percent of patients experience severe limitations in physical activities such as climbing stairs. 36 percent of them have problems with daily activities such as showering or dressing and 20 percent are hindered in social activities. These figures are three times higher than among the elderly who do not have a disease or condition.
3 When should you go to the doctor?
“Nothing to worry about”, many people will think with everyday complaints such as fatigue, shortness of breath, tickling cough and poor sleep. Or: “It must be because I am getting older.” For example, heart failure can remain hidden for a long time, while the patient starts to feel worse and worse. And that while the complaints can often be significantly reduced with good medication and an adapted lifestyle. In short: if you suffer from one or more of the above complaints, go to your doctor.
4 What is the prognosis?
Of the heart failure patients who only have symptoms when they exert themselves, 20 percent die within one year and 50 percent within five years. For patients with complaints at rest, the risk of death within one year is even 65 percent. It does not matter what the underlying cause of the heart failure is for the prognosis.
5 Is heart failure common?
Yes. About 35,000 people suffer from heart failure every year. In total there are now about 180,000 patients in the Netherlands. About 25,000 of them are hospitalized every year.
The number of people with heart failure is expected to increase significantly in the coming years. That’s because we’re living longer and because there are more and more people with diabetes, COPD (chronic bronchitis or emphysema) and serious obesity – they are at high risk of diseases that can lead to heart failure. In addition, a heart attack is fatal in fewer and fewer cases due to better treatment options. That means: more people with damaged heart muscle and therefore more patients.
6 When do you run extra risk?
People who live an unhealthy lifestyle – smokers, drink excessive amounts of alcohol, exercise little or are much overweight – have a higher risk of high blood pressure or a heart attack and therefore heart failure. Diabetics are five times more likely to develop heart failure than non-diabetics, while people with COPD are three to four times more likely. Incidentally, one in five patients whose GP has diagnosed COPD actually has heart failure. Their shortness of breath is often mistakenly attributed to COPD.
7 Do the symptoms get worse over time?
Yes. In a damaged heart, the remaining heart cells have to work extra hard to keep things going. Due to this overload, the healthy muscle cells are slowly but surely also damaged. Complaints such as fatigue and shortness of breath will therefore worsen in the long run. The rate at which this happens depends, among other things, on the effectiveness of the treatment and the general condition of the patient. Extra stress on the heart, for example in the form of a severe flu or pneumonia, can suddenly make the situation worse.
8 From what age can you start suffering from heart failure?
The majority of patients are older than 70 years. The risk increases with age. Between the ages of 45 and 65, three in a thousand people suffer from heart failure. Among the over-75s, there are ninety out of a thousand.
9 Is heart failure treatable?
Yes, but the damage to the heart muscle is usually irreversible. The treatment is then aimed at reducing the complaints and preventing the pumping function of the heart from further deteriorating as much as possible.
There are different types of medicines for the treatment of the complaints. The most important are water tablets, which drain the excess fluid, and drugs that work on blood pressure and on the pumping capacity and rhythm of the heart.
Furthermore, patients should learn to live a sensible and healthy life. They usually learn how best to approach this at the hospital’s special heart failure outpatient clinic. Often a combination of medication and an adapted lifestyle is sufficient. Sometimes it is necessary to implant a bilateral pacemaker, which ensures that the left and right ventricles continue to contract simultaneously.
Patients who do not respond well to treatment in the form of a healthy lifestyle and medicines or surgery may need a heart transplant in extreme cases. However, due to the limited number of donors, only a few people per year are eligible for this.
10 What should you pay attention to during treatment in hospital?
The care provided to patients with heart failure varies from hospital to hospital. That is why De Hart & Vaatgroep – the patient association for people with cardiovascular disease – has drawn up a list of criteria that good heart failure care must meet. This states, among other things, that at least two heart failure nurses must be working in the hospital and that the opportunity to participate in a special rehabilitation program must be offered. Patients can take this list with them when they talk to their doctor about treatment. For more information: www.hartenvaatgroep.nl or call 088-111 16 00.
11 Who can best treat you?
In most cases, a general practitioner makes the provisional diagnosis. Additional cardiological examination in the hospital is then necessary to determine whether there is actually heart failure and to trace the underlying cause of the complaints.
All hospitals now have a special heart failure clinic. The first point of contact at the heart failure clinic is a specialized nurse. Under the supervision of the cardiologist, he or she finds out which dose of medication is best for the patient, gives advice on exercise and diet, identifies whether the complaints are getting worse and adjusts the treatment in good time. Where necessary, there is collaboration with other specialties in the hospital and with the general practitioner or home care.
12 How does heart failure affect daily life?
Heart failure is drastic: patients have to learn to live with the knowledge that they have a (high) chance of dying quickly, they have to take into account that they are physically less able, that they have to take medication and that they are no longer allowed to eat and drink everything.
Because their bodies retain a lot of fluid, patients are advised to drink no more than two liters per day (including products such as yogurt and soup). If they drink more, their complaints often get (much) worse. This is a difficult lifestyle for many patients.
Patients with serious complaints are sometimes allowed to drink no more than 1.5 liters per day and are given a low-salt diet, with a maximum of 3 to 6 grams of salt per day. In comparison: the average Dutch person naturally only gets 9 to 10 grams of salt per day through their diet (so without addition from the salt shaker).
Alcohol is allowed, but in moderation. A maximum of two glasses a day for men, one for women. In larger amounts, alcohol further affects the damaged heart muscle. Anyone who smokes should definitely stop. Smoking reduces blood flow to the heart muscle.
Patients would do well to exercise on a daily basis. This ensures better blood circulation in the body and a good general condition. It is important to choose a form of exercise that does not suddenly put a lot of strain on the heart.
Many heart failure patients worry whether sex is not too much of a burden on their heart. In terms of effort, making love can be compared to climbing stairs. For patients who are well placed on medication and who can climb stairs at a reasonable pace (about twenty steps in a row in 10 seconds), sexual activity is not a problem.
13 What can we expect from new developments?
Doctors are increasingly able to detect heart failure at an early stage. This is done, among other things, on the basis of certain substances in the blood, so-called markers, which can indicate problems. More and more of those markers for heart failure are being found. The techniques for making an ultrasound or an MRI of the heart are also becoming increasingly precise.
Research into new treatment methods is still in its infancy. Until recently, doctors thought that the pumping function of a damaged heart muscle decreased because it became less powerful. It has recently been discovered that it is not the strength with which it contracts, but the flexibility of the heart muscle that is decisive. That means that scientists have to look for the solution in a different angle. New drugs may be able to increase the flexibility of the heart muscle in the future. It is also being investigated whether stem cells can replace damaged heart muscle tissue with healthy heart muscles. To date, this has not been successful.
One area where rapid progress is being made is home care for patients. A number of hospitals already offer a so-called health buddy. This is a system in which the patient carries out all kinds of checks at home and is in contact with the nurse via a device, who can then provide advice remotely based on the results.
TIP
You can order two brochures and a CD-ROM about (living with) heart failure free of charge from the Dutch Heart Foundation. T 0900-300 03 00 (local rate) or www.webshop.hartstichting.nl
TIP
Also read the heart special and take the test ‘Do I have a heart disease?’ at www.plusonline.nl/hart
This article was produced in collaboration with Dr. Jean Bronzwaer, interventional cardiologist and education coordinator of the cardiology department at the VU University Medical Center in Amsterdam. In 2003 he obtained his doctorate cum laude for a study which showed that it is not so much the lack of strength as the lack of flexibility of the heart muscle that can lead to heart failure.
Sources):
- Plus Magazine