On the occasion of World Alzheimer’s Day, Pourquoi Docteur takes stock of the diagnostic process for this pathology in France.

- In France, the system does not provide for systematic screening of the general population for the reason that there is no curative treatment for Alzheimer’s disease.
- Diagnosis is based on symptoms and biomarkers of the disease.
- In the United States, anyone with biomarkers for Alzheimer’s disease is considered sick, even without the presence of symptoms.
In 2024, the diagnosis of Alzheimer’s disease is still too late.National recommendations, currently being developed by the Federation of Memory Centers, aim to improve this processindicates the Overcoming Alzheimer’s Foundation in a press release sent to the editorial staff. It is important to strengthen in particular the identification in general medicine, the time taken to refer patients to Memory Consultations and to carry out examinations, raising public awareness of the benefits of a diagnosis made as early as possible, and the training of health professionals.”
How is Alzheimer’s disease diagnosed in France?
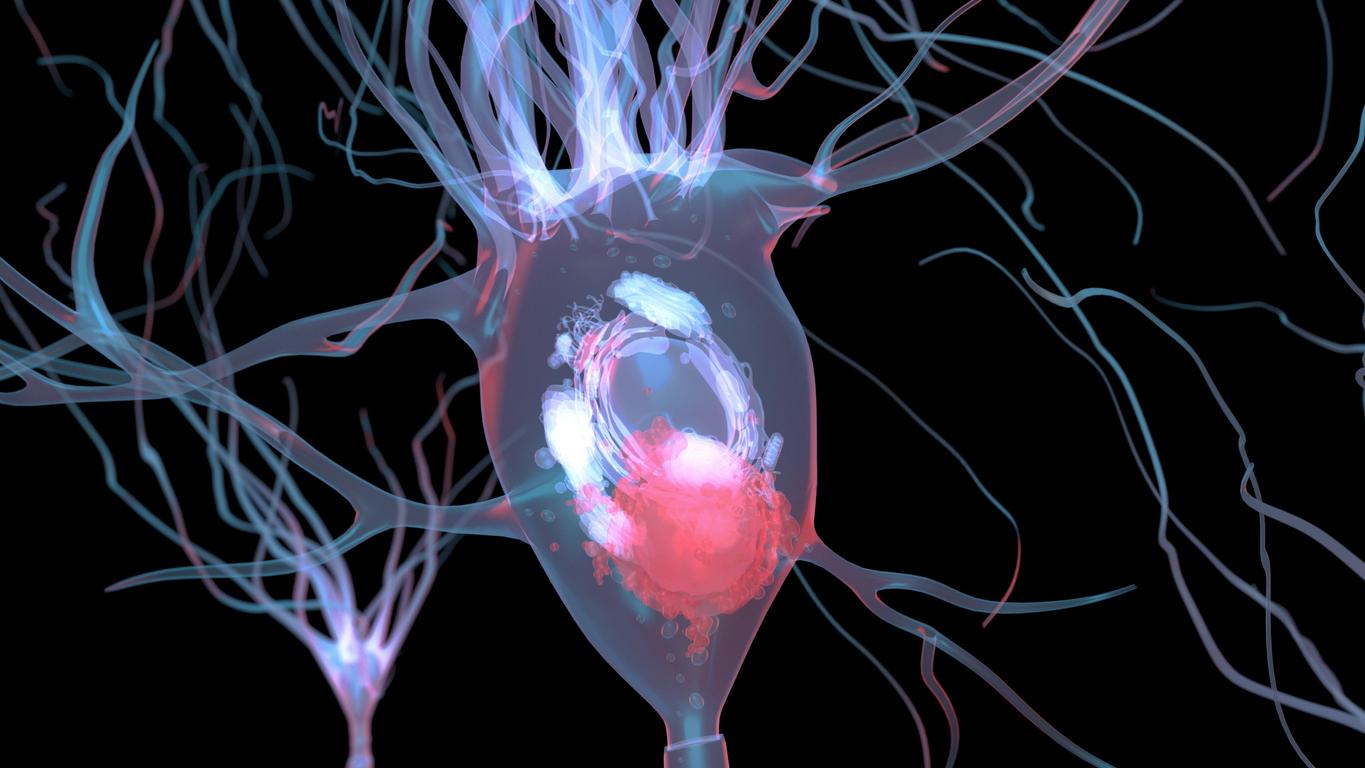
In France, the system does not provide for systematic screening of the general population because there is no curative treatment for Alzheimer’s disease. Thus, screening focuses only on patients with specific symptoms. As such, the role of the general practitioner is essential because it is he who can detect early signs of disorders and, as a result, refer the patient to specialized care and examinations (brain MRI, blood test, thyroid ultrasound, neuropsychological tests, etc.). These examinations make it possible to know whether the patient has a curable disease that can cause cognitive disorders or a neurocognitive disease. In France, the diagnosis of Alzheimer’s disease is therefore based on the symptoms and biomarkers of the pathology.
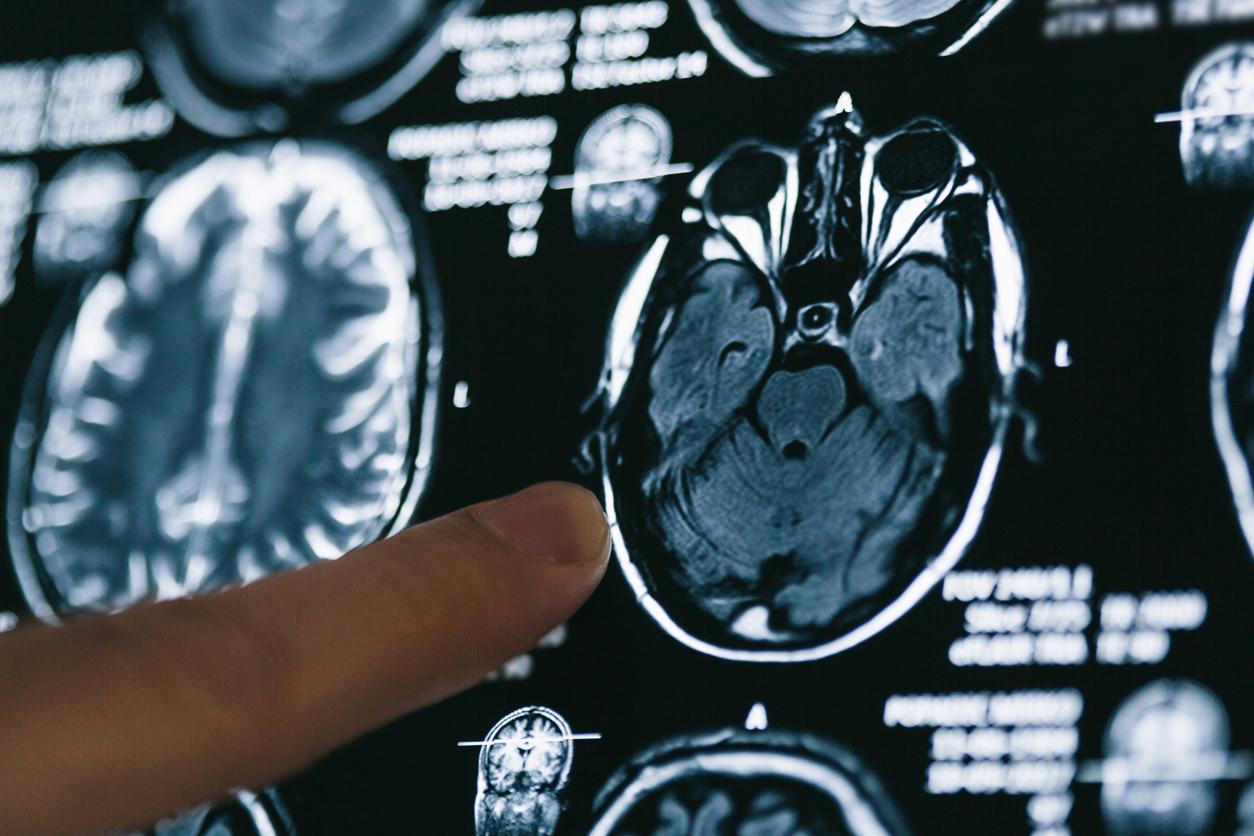
Alzheimer’s: a diagnosis based solely on biomarkers in the USA
On the other side of the Atlantic, it’s a completely different story. This is partly because in the United States, medicine has always been studied from a more “biological” perspective than in Europe, and this has repercussions on health regulations.In Europe, it is considered that carrying a genetic mutation – which could potentially make you sick if you live long enough – does not mean that you are already sick.“, explains Professor of Neurology David Wallon, who directs the Memory Resources and Research Center at Rouen University Hospital and co-director of the National Reference Center for Young Alzheimer’s Patients for the diagnosis and specific care of Alzheimer’s disease in young people, particularly genetics.On the other hand, in the United States, being a carrier of a mutation is enough to be classified in a category of individuals considered to be affected by a pathology. From a regulatory point of view, there is an obligation to declare one’s status in many insurance contracts. This is not the case in France, where a genetic result is not an element justifying a declaration in a medical certificate for insurance. (…) Concerning the diagnosis of Alzheimer’s disease, it is a bit the same thing: in the United States, as soon as brain lesions are detected in the brain (thanks to the positivity of biomarkers) the Alzheimer’s Association considers that the person is sick, even in the absence of symptoms. However, it is entirely possible to live one’s entire life with brain lesions without developing Alzheimer’s disease during one’s lifetime.“This is confirmed by Professor Lea Grinberg, who works at the Memory and Aging Center at the University of California, San Francisco (UCSF) and the University of São Paulo: “(…) not all individuals who accumulate amyloid will systematically experience clinical decline. Should they then be subjected to expensive and invasive treatments? Furthermore, basing a diagnosis solely on imperfect tests (because all these biomarkers remain very imperfect with respect to neuropathology) is a risk of ignoring the need for a clinical assessment. We would end up treating people on the basis of an examination, and not on that of a holistic approach to the disease.”
Alzheimer’s disease: the 10 main areas of research on diagnosis
According to the Vaincre Alzheimer Foundation, we have ten avenues of research available on the diagnosis of Alzheimer’s disease in order to speed up the process and improve patient care:
- multimodal imaging;
- the help of artificial intelligence;
- retinal imaging;
- the PET Scan;
- electroencephalogram;
- digital tools;
- eye tracking;
- the use of bodily fluids: blood, cerebrospinal fluid and other biological fluids such as urine or tears.
“The development of blood biomarkers, digital tools and AI models will make it possible to identify the best responders to treatments, while minimizing secondary risks.”, she says.However, the current lack of financial resources is holding back this progress, both in the private and public sectors. But the arrival of future treatments could raise hopes of a revival of financial support from investors, particularly for private structures, in favour of the development of new methods of early diagnosis.”
Each year in France, 225,000 new cases of Alzheimer’s disease are diagnosed, but the Foundation specifies that one in two patients is not diagnosed or is poorly diagnosed.