Scottish researchers have developed a new therapy against tuberculosis that would reduce the duration of medical treatment to two months.
- Tuberculosis is transmitted through the air via droplets containing the infectious agent and coughed up by patients.
- Scientists from the University of St Andrews (Scotland) have unveiled a new drug therapy that could reduce the duration of treatment for tuberculosis.
- The clinical trial observed the efficacy of BPaMZ therapy in patients with drug-susceptible or drug-resistant tuberculosis.
In 2020, the World Health Organization reports that nearly 1.5 million people died from tuberculosis, making it the 13th leading cause of death and the 2nd due to an infectious disease globally. This pathology is caused by Koch’s bacillus, an infectious agent that is transmitted through micro-secretions emitted when an infected person coughs or sneezes.. “It is a disease usually prolonged for several months”warns the Ministry of Health and Prevention.
Shortened duration of tuberculosis treatment
To treat tuberculosis, several antibiotics are usually prescribed to patients for at least six months. If the treatment is followed well, the patient recovers without difficulty, but resistance to anti-tuberculosis drugs can occur when it is not taken correctly.
At the time of the 30th Annual Conference on Retroviruses and Opportunistic Infections (CROI)in Seattle (United States), researchers from the University of St Andrews (Scotland) have unveiled the promising results of a new drug therapy that would shorten the duration of treatment for tuberculosis to two months and save million patients.
The Global TB Alliance’s SimpliciTB clinical trial evaluated BPaMZ therapy consisting of several anti-TB drugs (bedaquiline, pretomanid, moxifloxacin, pyrazinamide).
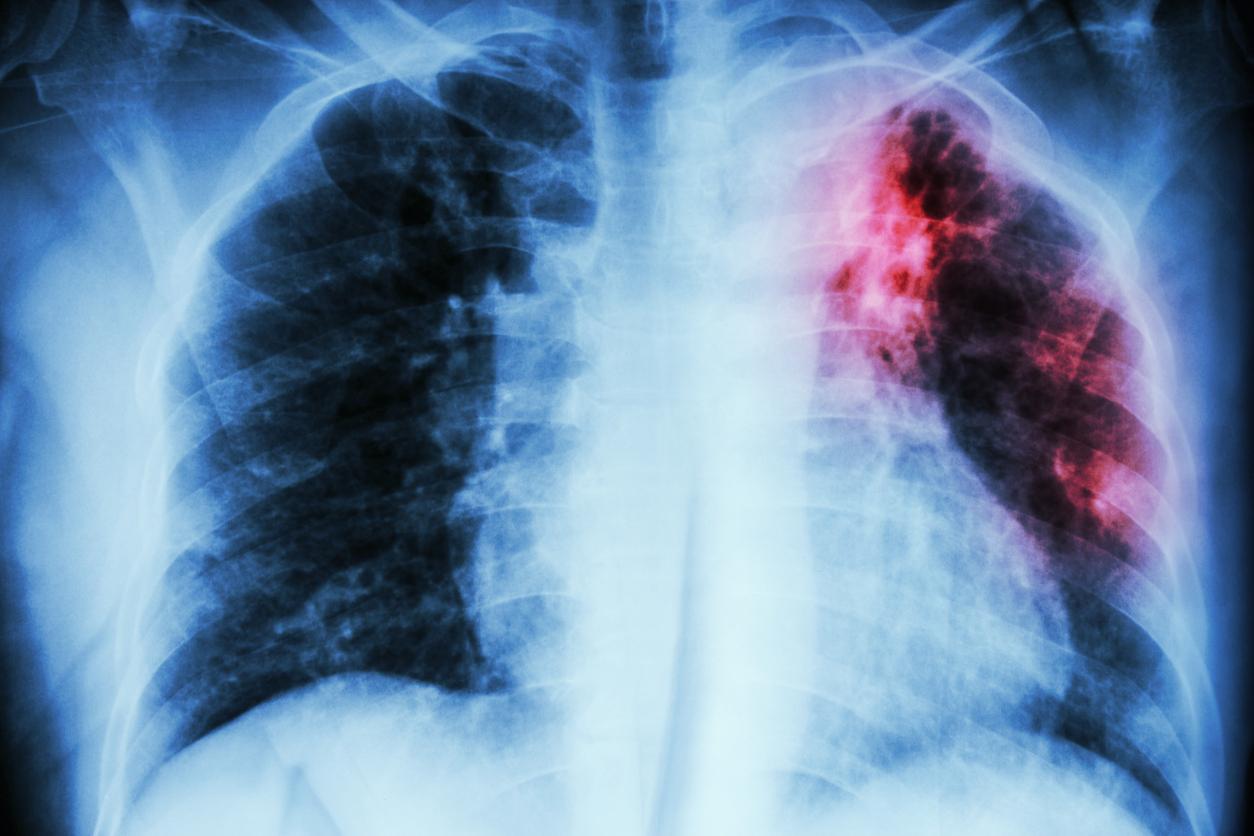
Tuberculosis: effective therapy against drug-sensitive and drug-resistant forms
For this research, scientists recruited 455 patients with drug-susceptible or drug-resistant tuberculosis to observe the safety and efficacy of BPaMZ therapy in these patients.
According to the results, the BPaMZ therapy was very potent against Koch’s bacillus, which causes tuberculosis. Participants with drug-susceptible TB were 2.93 times more likely to see their condition improve after two months of treatment.
“Innovative clinical trials like SimpliciTB are helping us better understand how new drug therapies work against both drug-susceptible and drug-resistant TB, illuminating the way to better treatment options for all TB patients,” noted Dr. Muge Cevik, research author and clinical scholar in infectious diseases and medical virology at the University of St Andrews Medical School.
In the coming months, the Global TB Alliance will submit the results of its clinical trial to a peer-reviewed and peer-reviewed publication.