New research from Finland suggests that excessive use of certain antibiotics could increase the risk of Parkinson’s disease, with a delay of 10 to 15 years. This link can be explained by their disruptive effects on the microbial ecosystem of the intestine.

Antibiotic resistance, also called antibiotic resistance, is a major health scourge. Each year in France, 125,000 infections and 5,500 deaths are linked to it, according to Inserm data.
This phenomenon, which designates the resistance of “super bacteria” to antibiotic drugs administered to treat many infections, is linked to an excessively systematic and massive use of these treatments.
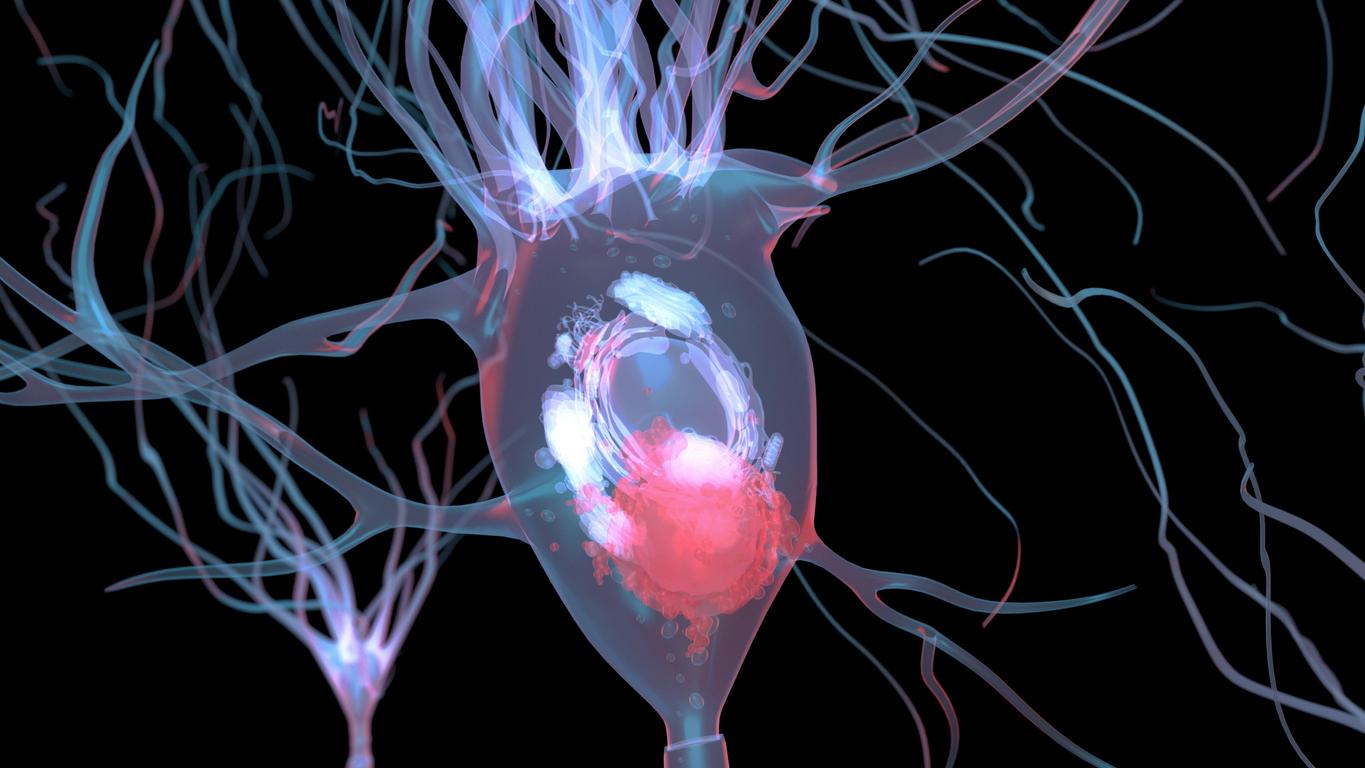
But these resistant infections would not be the only negative effects of the abuse of antibiotics which could be involved in neurodegenerative diseases.
Thus, in order to measure the rate of incidence of exposure to antibiotics (taking into account the duration) on the risks of developing symptoms of Parkinson’s disease, a new study published in Movement Disorders focused on all patients diagnosed with Parkinson’s in Finland between 1998 and 2014.
First signs 15 years before Parkinson’s diagnosis
Information about individual purchases of oral antibiotics during the years 1993 to 2014 from these patients was collected as part of the research.
In total, the study identified 13,976 Parkinson’s cases and 40,697 unaffected controls matched by age, sex and place of residence. The strongest associations were observed for broad-spectrum antibiotics and those that act against anaerobic bacteria and fungi.
Antibiotic exposure was examined over three different time periods: 1-5, 5-10, and 10-15 years before the date of diagnosis, based on oral antibiotic purchase data. Exposure was classified according to the number of drugs purchased, the class of antibiotics according to their chemical structure, their antimicrobial spectrum and their mechanism of action.
“The structure of the associations supports the hypothesis that effects on the gut microbiota may link antibiotics to Parkinson’s disease, but further studies are needed to confirm this hypothesis,” the study authors conclude.
.