Rheumatoid arthritis, an autoimmune disease that attacks the joints, may be caused by a unique bacteria in the gut microbiome, according to a new study.

- Rheumatoid arthritis is a chronic autoimmune inflammatory disease that attacks the joints and manifests itself in flare-ups. It would concern around 300,000 people in France. Current treatments do not allow cure but remissions or relief of symptoms.
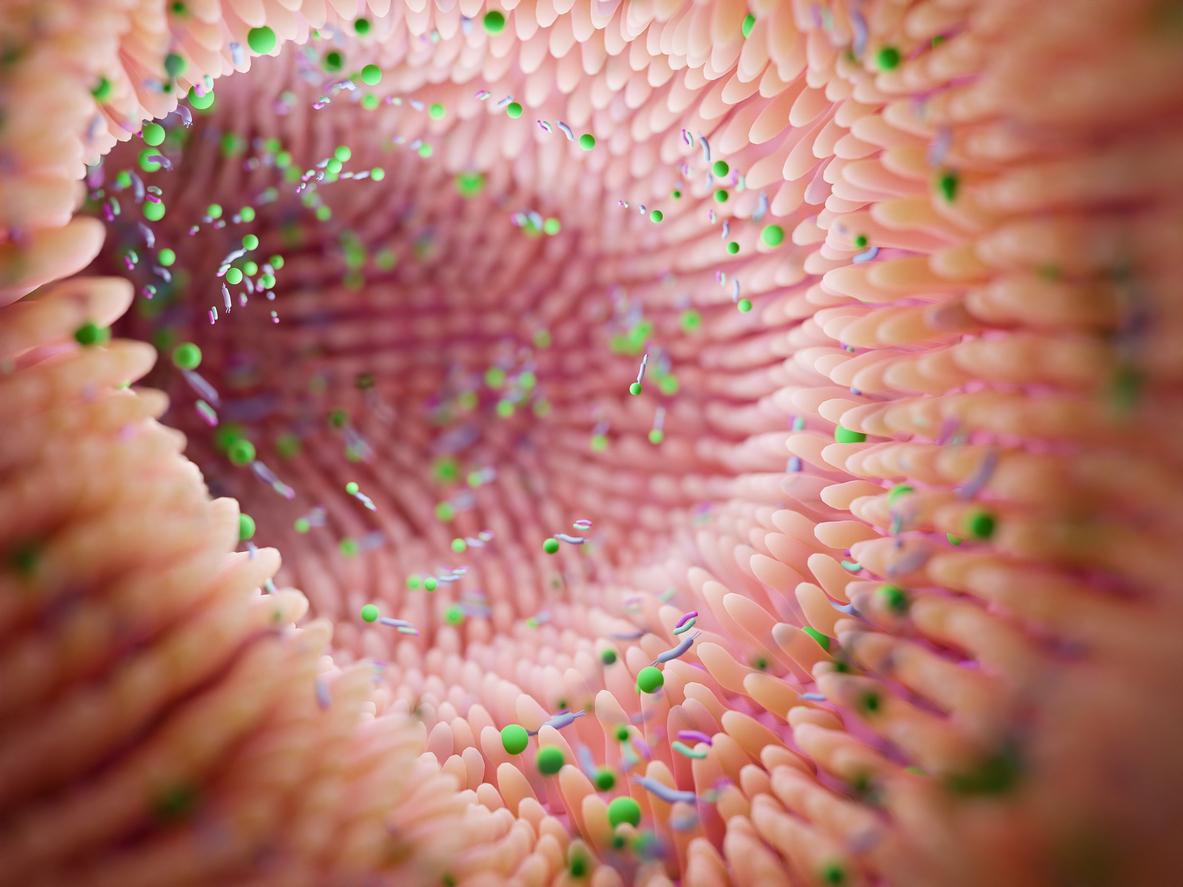
- The intestinal microbiota is a set of microorganisms, mainly bacteria in our digestive tract. In total, more than 100,000 billion bacteria of more than 400 species are present in the intestinal flora. In association with the intestine, it plays an important role in digestion.
Researchers at the University of Colorado School of Medicine have found that a unique bacteria found in the gut may be responsible for triggering rheumatoid arthritis (RA) in people already at risk for the autoimmune disease . Their work has been published in the journal Science Translational Medicine.
As a reminder, rheumatoid arthritis is an autoimmune disease (that is to say resulting from a dysfunction of the immune system) which attacks the joints. Some 300,000 people would be affected in France. And current treatments don’t provide a cure, only remission or symptom relief.
A single bacterium causing rheumatoid arthritis?
As part of their research, which took five years and required many volunteers, the scientists first established that people at risk of RA could be identified by antibodies present in the blood, several years before the diagnostic. By sifting through them, they observed two different types of antibodies: classics, those normally seen in circulation, and antibodies “generally associated with our mucosa, whether oral, intestinal or pulmonary”explains in a communicated Kristine Kuhn, professor of rheumatology in charge of the research team. “We started thinking, ‘Could there be something in the mucous membrane that could be causing rheumatoid arthritis?'”
To support their hypothesis, the researchers mixed these antibodies from individuals at risk of contracting the disease with the feces of the same people at risk. The objective, to identify the bacteria marked by the antibodies. They then used animals to host these newly discovered bacteria. And their work paid off: “These experiments showed that not only did the bacteria cause the animal models to develop the blood markers found in individuals at risk for RA, but some of the models also showed the development of full-blown RA”can we read in the study.
Hope to predict who will develop this autoimmune disease
According to Kristine Kuhn, if the single species of bacteria is indeed at the origin of the immune response which leads to rheumatoid arthritis in people already at risk of contracting the disease, it might be possible to target the bacteria with drugs to prevent this response from occurring.
The next step will therefore be “to identify, in larger populations of individuals at risk for RA, whether these bacteria correlate with other genetic, environmental, and mucosal immune responses, and then ultimately, the development of RA”, hopes the researcher. which concludes: “We could then say, ‘This is a useful marker for predicting who will develop rheumatoid arthritis,’ and apply prevention strategies.”