Tested in phase I and II, a new chemotherapy treatment comprising paclitaxel injected into the abdomen has been shown to be effective in patients with pancreatic cancer with metastases.

- A new combination of chemotherapy drugs has shown efficacy against metastatic pancreatic cancer, an aggressive and often fatal form of the disease.
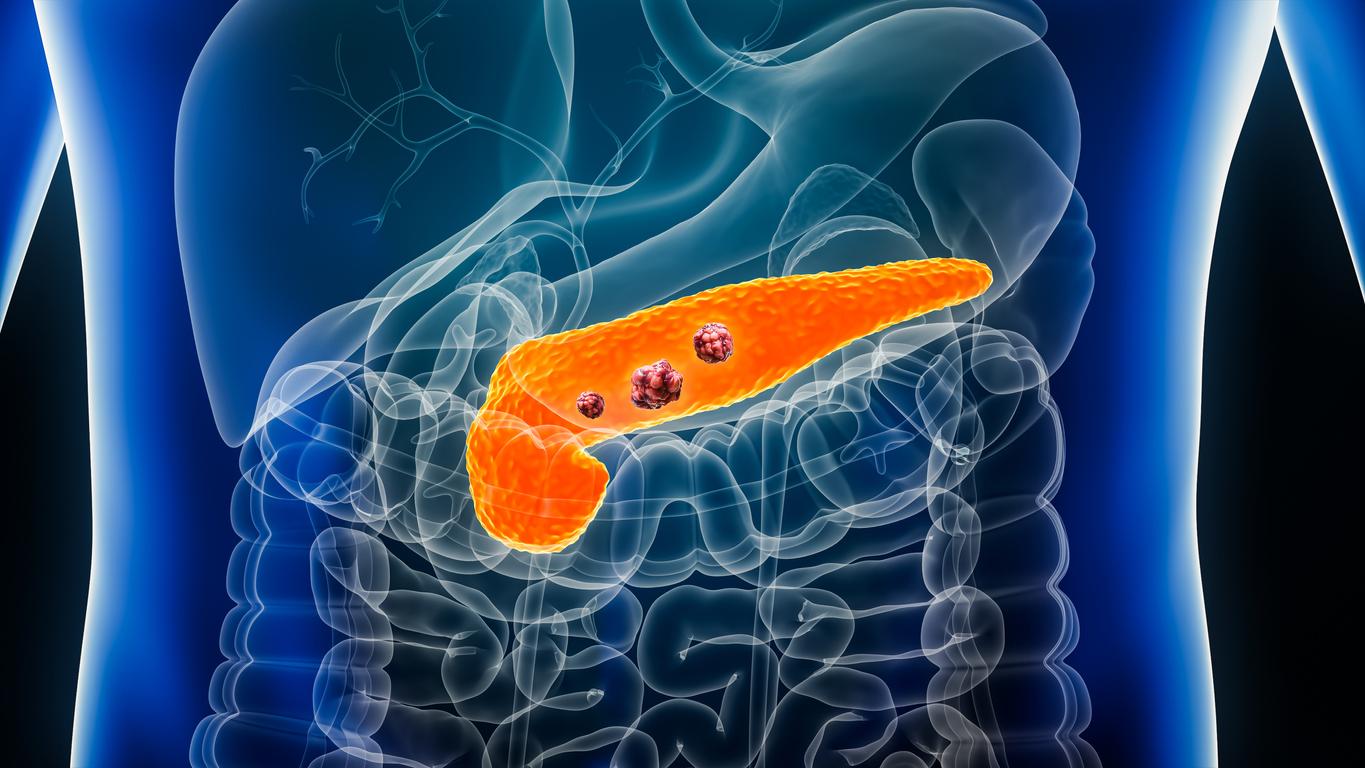
Rare but often aggressive, pancreatic cancer is characterized by the usually silent development of malignant cells on the pancreas, which eventually form a tumor, disrupting the functioning of the organ and its environment. Because it causes no recognizable symptoms in the early stages of its development, pancreatic cancer is also one of the deadliest. Every year, 300,000 people die from it worldwide. According to French National Society of Gastroenterology (SNFGE), 14,184 new cases of pancreatic cancer were detected in France in 2018, 50% of which were diagnosed at the metastatic stage. It caused 5,790 deaths.
A new study, published in the British Journal of Surgery may offer a better chance of survival for patients with metastatic pancreatic cancer. According to its authors, a new cocktail of chemotherapy drugs would prove effective in the fight against this aggressive form of pancreatic cancer.
An increased median survival time
Conducted in 46 patients, the phase I and II study tested the safety and efficacy of a cocktail of drugs: injunctions of paclitaxel in the abdomen (intraperitoneal injection) and injections of gemcitabine and nab- paclitaxel (a combination of paclitaxel and a protein called albumin) in the blood.
Treatment was repeated every 4 weeks until unacceptable toxicity developed, disease progression, or surgery. The advantage of intraperitoneal injection chemotherapy is that it allows tumors to be exposed to high drug concentrations without increasing the systemic concentration to toxic levels.
The results were positive: the patients had a median survival time of 14.5 months, with a one-year survival rate of 60.9%. As for the drug combination, it showed acceptable tolerability. Thus, hematological toxicities occurred in 35 of the 46 patients and non-hematological adverse events in seven. However, the researchers point out, the incidence and severity were comparable to those of standard chemotherapies.
“Now, a phase 3 study to compare survival outcomes between this therapy and standard chemotherapy has been launched.”said lead author Sohei Satoi, a researcher at Kansai Medical University (Japan).

.