The many advances that have been made in recent years in treatments will lead to even more benefits with new methods of evaluating the disease.
The recent increase in the number of different therapeutic combinations validated for patients with multiple myeloma is accompanied by a revolution in the evaluation of their effect on the disease and the level of remission. Accurate measurement of the depth of remission under these treatments paves the way for a complete redefinition of treatment goals.
Recent studies and analyzes show that negative minimal residual disease (MRD) is associated with longer progression-free survival and overall survival in patients with multiple myeloma. With the use of modern treatment strategies, over 60 percent of newly diagnosed multiple myeloma patients achieve complete responses and negative MRD.
There would be no small myeloma
New data indicate that between 90 and 95% of patients with an early form of early myeloma (“smoldering myeloma”) may obtain complete responses and negative MRD.
For Professor Ola Landgren, there is no form of myeloma that does not require treatment. It is not necessary to wait for clinical signs such as fractures or major spinal cord invasion to consider a person ill and treat them. All the data he presented in a controversial session at ASH suggests that the results of treatment in terms of residual tumor mass and duration of remission, are better the earlier the treatment and the more the tumor mass is low. He therefore suggests treating very early myelomas with the most effective treatments in order to try to eliminate the disease permanently.
At present, however, there is no evidence that this intensive early treatment strategy is able to completely eradicate the disease. Some experts point out that there is still a clone of tumor cells that are naturally resistant to treatment or become resistant and are likely to persist. A certain number of experts still believe that, for the comfort of the patients, it is better to treat the myeloma when it becomes progressive, even if it means following the trailing myelomas on markers more sensitive than the traditional clinical, biological and radiological signs in order to make a therapeutic decision before the tumor mass is too large.
The promises of minimal residual disease
Minimal residual disease, or MRD, is a concept that assesses the quality and depth of response to treatment.
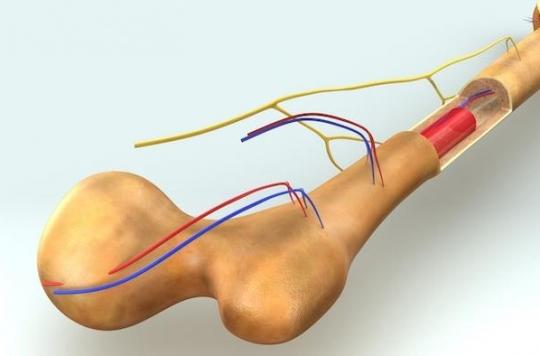
It is determined by ultra-sensitive techniques for detecting myeloma cells in the marrow. There are several techniques for assaying these cells, including new generation genetic sequencing, or NGS (“Next Generation Sequencing”), or a new standardized flow cytometry technique called “Next Generation Flow Cytometry”.
The sensitivity of these techniques is such that they are able to detect a single myeloma cell out of a million cells in the bone marrow. This threshold of 10-6, seems to be the threshold from which experts define a relevant bone marrow remission of the disease since this threshold is associated with a real difference in prognosis and survival.
This threshold is so discriminating that patients who are able to reach an MRD of 10-6 without any bone marrow transplants, the “nuclear weapon” of myeloma treatment, are able to have the same prognosis as those who have been transplanted. On the other hand, if we look at patients who have a lot of genetic abnormalities with a poor prognosis, those who reach a negative MRD have a much better prognosis than those who do not reach the threshold of 10-6. Finally, MRD is a dynamic concept that works whatever the stage of the disease and allows it to be monitored over the long term. Finally, the MRD at 10-6 is also a threshold which is associated with a significant increase in disease progression free survival (PFS), but also overall survival, that is to say the actual survival of patients.
A change in strategies
Advances in myeloma treatments currently pose a paradoxical problem for hematologists: extending overall survival and progression-free survival increases the duration and cost of studies in myeloma since the endpoint is currently relapse and this can take 7, 8 or 9 years. This extension of therapeutic trials until this term represents a debauchery of financial means and a loss of opportunity for many patients.
Next-generation sequencing which becomes accessible and the definition of MDR with a threshold of 10-6 make it possible to have an extremely sensitive biomarker which should make it possible, in future clinical trials, to adjust the treatment according to the minimal residual disease without waiting for clinical or biological relapse. This technique of NGS has a cost, of course, but if it makes it possible to diagnose very quickly that an expensive treatment does not make it possible to obtain an MDR or that the MDR goes back under this treatment, it is possible to stop it immediately and to change immediately to another more effective treatment. Likewise, if after any induction treatment, an MRD of 10-6 is reached, it can be discussed to do only one transplant and not 2, or even not to do a transplant at all, to reserve it for a later phase of the disease.
In view of the cost of new treatments and of the transplant, the cost for society is reduced and this avoids subjecting the patient to unnecessary treatments. Thus, we see emerging in myeloma the advent of a chronic treatment adjusted to each phase of the disease according to an MDR objective of 10-6. The assessment of the MDR will allow these early upward adjustments as soon as the disease recovers, just as it will allow periods when the patient will remain without maintenance treatment and under simple surveillance.
Re-discussion of extended maintenance treatments
In a presentation which closed this session, it appeared that it is not certain that these maintenance treatments are necessarily prolonged in all patients.
When we review the main therapeutic trials which have promoted long-term maintenance treatments with lenalidomide, for example, we see that they are very heterogeneous on the one hand (all the trials do not show any benefit), and that the benefit in terms of survival is modest and above all takes a long time to be expressed (it takes several years to see a significant difference). This phenomenon is all the more embarrassing given that lenalidomide in prolonged treatment is accompanied by an increase in secondary cancers.
In view of these data, the experts looked at the individual data of patients from the different studies and, by dividing the patients into more homogeneous groups according to different criteria of severity, they show that prolonged maintenance treatment with lenalidomide would not bring any benefit in patients without criteria of gravity. The benefit only appears in patients in good general condition who have poor prognostic factors (genetic factors, etc.). Here again, the use of MDR should make it possible to stop all maintenance treatment in patients in complete bone marrow remission since this technique will make it possible to resume treatment adapted to the slightest sign of resumption of the disease in the marrow.
The past 10 years have been exciting and hopeful for myeloma sufferers and what lies ahead is even more exciting. We now have a lot of high-performance molecules and new tools are arriving to allow us to make the best use of them. After having more than doubled the life expectancy of patients suffering from myeloma, this hemopathy gradually becomes a chronic disease and the cure of some patients becomes possible.
.