This can be done
Heartburn is a common problem. The solution is not only in medicines. Simple rules of life also reduce the complaints.
Heartburn is often caused by a malfunctioning sphincter between the stomach and esophagus, and an opening in the diaphragm that is too wide, causing the stomach to rise slightly into the chest cavity (gastric hernia or hernia). The risk of this increases with age, smoking and obesity.
This poorer sealing function allows acid to flow back from the stomach into the esophagus. This is called reflux, or ‘backflow’. The stomach wall is lined with a thick mucous layer and thus is well protected against the acid, but the esophagus does not have such a protective layer and becomes irritated or even inflamed if stomach acid gets into it. That can hurt a lot. The burning sensation behind the sternum is sometimes even mistaken for heart problems.
simple pill
For occasional complaints, antacids can be purchased without a prescription at the supermarket, drugstore or pharmacy. These are usually agents that bind the stomach acid for a short time, such as calcium or magnesium carbonate, or gastric acid inhibitors (ranitidine or cimetidine) in a low dose.
Stronger Medicines
The GP can prescribe different types of medicines that are stronger than the over-the-counter medicines. Some apply a protective layer to the mucosal lining of the esophagus and stomach, others promote the functioning of the esophagus and stomach muscles.
Between 80 and 85 percent of people with reflux symptoms can taper off the acid-blocking drugs after about eight weeks. However, many people take them longer than necessary. Discuss with your doctor or pharmacist when you can start tapering.
Operation
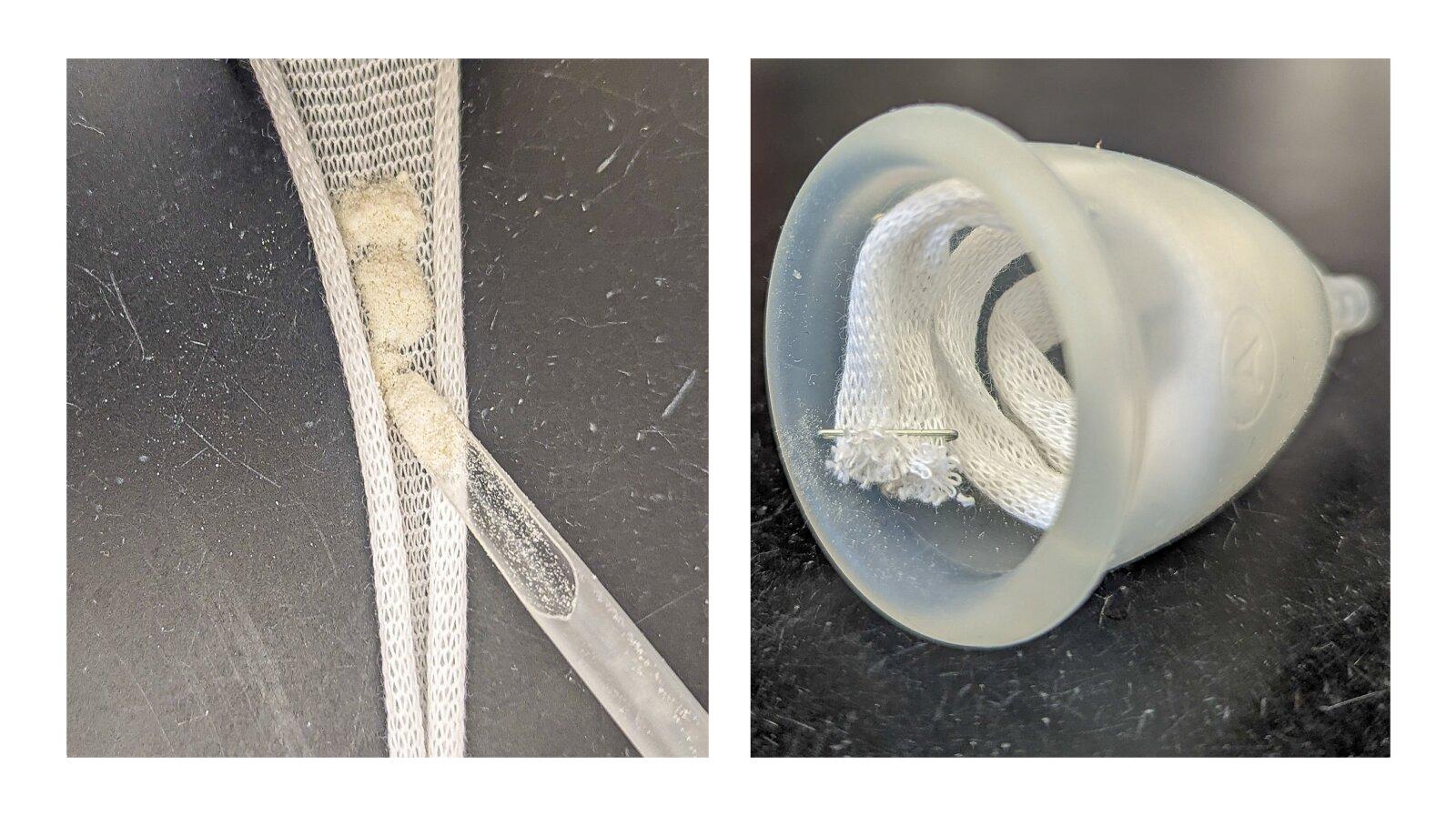
Medicines do not help for a small proportion of people. They are eligible for surgery to repair a diaphragmatic hernia. This is about 5 percent of the cases. During surgery, the top of the stomach is wrapped around the wall of the esophagus and secured. This restores the closing function of the stomach.
The choice between medication and surgery is determined on an individual basis. The AMC is the only Dutch hospital to have an outpatient clinic (MOT-CHIR) that specializes in reflux complaints.
Do it yourself
- Avoid fatty foods, as they stay in the stomach longer.
- Be careful with alcohol, peppermint, chocolate, coffee, spicy herbs and carbonated drinks and with acidic fruit juices from citrus fruits such as grapefruit and orange.
- Do not consume very cold or hot foods or drinks.
- Prevent intestinal blockage, because full intestines put more pressure on the stomach. Eat high fiber, drink at least 1.5 to 2 liters of fluids daily and exercise a lot.
- Do not take copious meals. It is better to have a small meal more often during the day.
- Do not eat shortly before and after physical exertion.
- Do not eat at least three hours before going to bed so that your stomach is empty when you lie down.
- Eat at a leisurely pace and in a good atmosphere, and chew well.
- Stop smoking, because smoking relaxes the sphincter between the esophagus and stomach.
- Try to lose weight if you are overweight, because excess pounds push the stomach up.
- Do not wear clothes that pinch around the stomach.
- Raise the head of the bed a little; that prevents stomach contents from flowing back into the esophagus at night. A thicker pillow is counterproductive, because it actually puts the stomach more in a pinch.
- Avoid bending over just after eating. Kneel and keep your torso upright if you need to pick something up.
- Reduce stress, because this causes the stomach to produce more acid.
To the doctor
See your doctor if you still have symptoms after a few weeks despite the over-the-counter medication. He may refer to an internist or specialist for a gastroscopy. An endoscope (a viewing instrument attached to a tube) is then used to look at the inside of the esophagus and stomach. X-rays or a 24-hour acidity measurement can also clarify what the problem is.
Go back to the doctor if the symptoms persist. If the lining of the esophagus is exposed to stomach acid for a long time, people can develop what is known as Barrett’s esophagus: a permanent change in the esophageal tissue. About 10 percent of Dutch adults with long-term and daily reflux symptoms have this. 1 percent of them develop (an aggressive form of) esophageal cancer, a so-called adenocarcinoma. This form of cancer has increased by 600 percent in the past forty years, partly because obesity is more common. In people with Barrett’s esophagus, troubled cells, which indicate a precancerous stage of cancer, can be cut and/or burned. The esophagus then recovers.
This article was produced in collaboration with Dr Jacques Bergman, professor of gastro-intestinal endoscopy at the AMC-UvA.
Sources):
- Plus Magazine