Make your own chemo plan!
The diagnosis of cancer takes away all the ground from under your feet in one fell swoop. Fear and uncertainty play a major role in this. Your own chemo plan helps you to prepare for the treatments and to go through the chemotherapy as well as possible. Because it is nice if you know in advance what to expect.
Everyone knows someone with cancer. An elusive condition that comes in many shapes and sizes. Chemotherapy is the appropriate treatment for many cancer patients, whether or not in combination with, for example, radiation. A so-called chemo plan is useful in preparing for the treatment process and helps to map out the possible physical and emotional consequences of this far-reaching disease.
Your chemo plan will be used before, during and after chemotherapy. It describes the details of specific rules and agreements or the treatment schedule, gives you an overview and shows you what to expect from the treatment. Such a plan can be made online via Chemotherapie.nl. You develop a good plan together with your doctor and oncology nurse and includes:
• A schedule of your treatment
• A list of the types and amounts of medicines you receive
• A description of the possible physical and emotional side effects
• A checklist of signs that tell you when to call your doctor or oncology nurse
• A list of phone numbers and times to reach your doctor or oncology nurse
• Approach and options to prevent side effects or make them manageable
• What you can do at home and how your environment can help
• Flexible and realistic objectives
• A list of resources that provide you with information and support
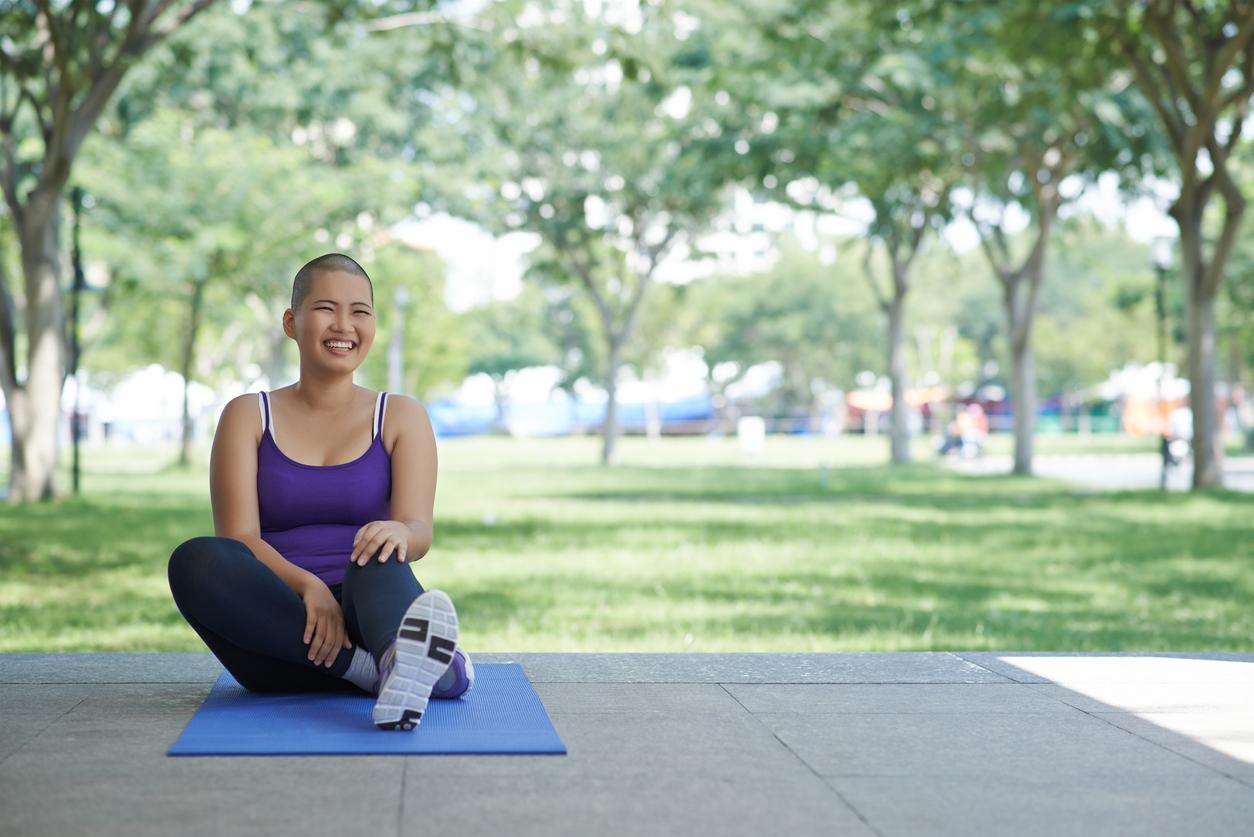
body & mind
Because the diagnosis of cancer has far-reaching consequences both physically and mentally, it is advisable to take this into account in your step-by-step plan. Therefore, make a distinction between body and mind at the start of the chemo plan; in other words: body and mind. In addition, set aside space to keep a journal. this does not have to be very extensive, but in any case note any side effects or mood swings at each step in the treatment process. For example, do you have a fever? If you have a fever above 38.5 degrees Celsius, you should call your doctor right away to avoid a high fever and/or infection. Then you not only have the contact details at hand, but the doctor can also follow the course of the disease exactly.
Body
In the body section of your chemo plan, in addition to the ‘normal’ information about the treatment process, you also list for yourself which questions and subjects are extra important to you. For example, take a good look at the side effects other cancer patients experience during chemotherapy and whether you have any questions about this. Your doctor and oncolology nurses can answer any questions you may have and will know who to turn to if they don’t have a ready-made answer.
Do not only think of side effects such as nausea, listlessness or weight loss and possible solutions against them, but also write down for yourself what you would think about it, for example if your hair were to fall out. In your case, are there treatments with less chance of hair loss? Are you going to buy a wig and if so, how much will the insurance reimburse and where will you do that? What should this wig look like? Other questions may include: Would you like pictures of your body before treatment? Can a manicure help with the chemo side effects? Do certain foods help prevent nausea?
Spirit
Chemotherapy leaves not only physical marks, but also mental scars. It affects your memory and concentration, but also affects your mood. Cancer and chemotherapy can make you feel anxious and insecure. Sometimes depressive feelings arise. And of course there is Area – a partner, (grand)children, friends – who are worried about you and who are having a hard time. Talking about it is sometimes difficult, but very necessary.
In addition to the oncology nurses and the specialist, there is a whole army of people who can help inform the environment, process feelings and talk about all possible issues that you encounter during treatment. This also includes psychologists, support groups and organizations such as ‘Looking good, feeling better’ (formerly ‘Well-groomed, better feeling’), the Breast Prostheses Information Center (BIC) or, for example, the Tophaarwerkersgilde Nederland.