What to remember from the two years of the pandemic? Elements of response with Pr Claire Andréjak, pulmonologist at the University Hospital of Amiens-Picardie.

- 21,169 patients are currently hospitalized for Covid-19 and 3,759 people are in intensive care.
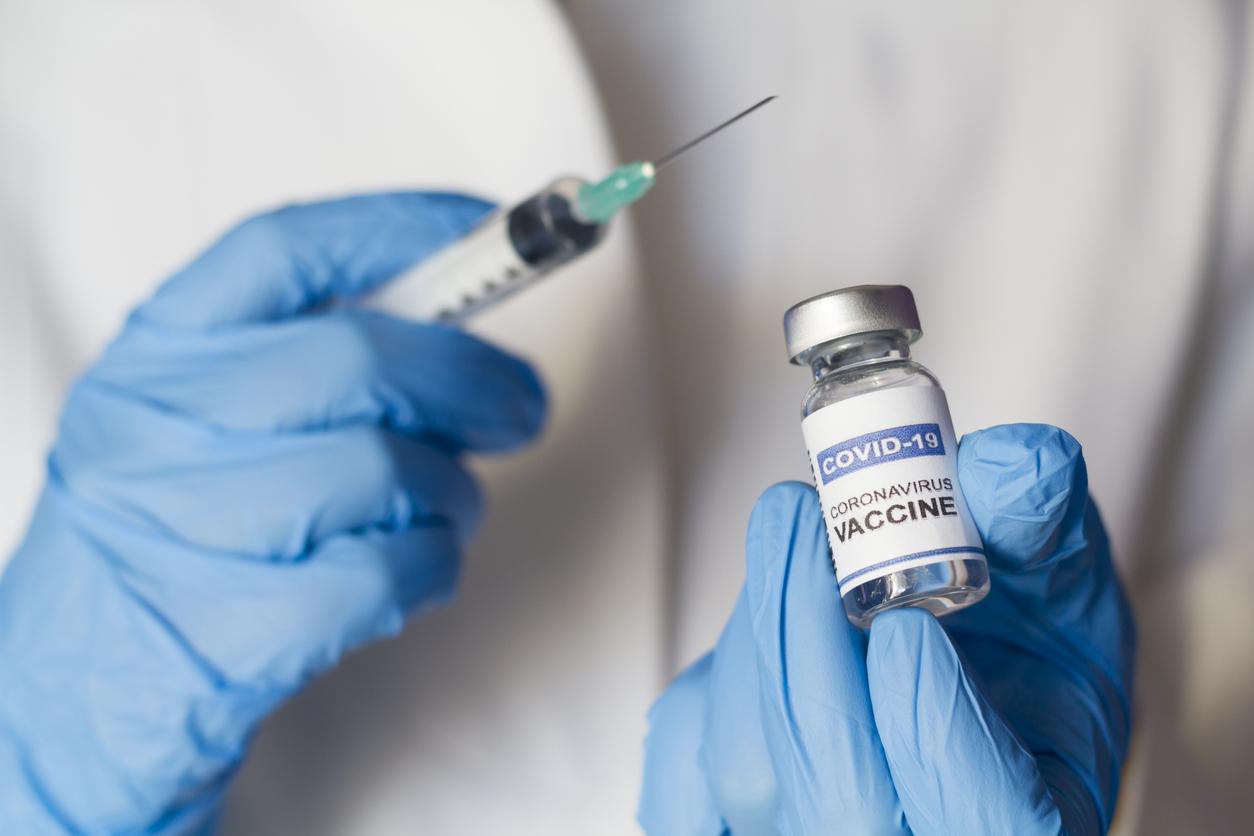
- Since the start of the anti-Covid vaccination campaign in France, 53,123,626 people have received at least one injection (i.e. 78.8% of the total population) and 51,916,583 people now have a complete vaccination schedule (i.e. 77% of the total population).
During a press conference preceding the 26th edition of the CPLF, Pr Claire Andréjak, pulmonologist at the University Hospital of Amiens-Picardie and head of a research group in pneumo-infectiology (GREPI), took stock of two years of health crisis.
“Without vaccines, the hospital would be dead”
The year 2021 was of course first marked by the arrival of anti-Covid vaccines. “They may not be perfect, but they have changed the game, protecting serious forms and limiting contamination”, recalls Claire Andréjak. “If we hadn’t had these vaccines today, the hospital would be dead”, continues the specialist.
“Monoclonal antibodies are effective”
Regarding treatments for the coronavirus, “monoclonal antibodies have revolutionized care, especially for people who do not respond to vaccination. They are effective against the majority of variants, except unfortunately for Omicron. They will therefore not be used in the latter case”, explains Claire Andréjak.
“Promising new molecules”
In addition to monoclonal antibodies, new curative molecules* are or should soon arrive on the market. “They are promising, but to be effective, they must be administered very early, which implies a particular organization, in particular at the level of the tests”, believes the pulmonologist. “It will also be necessary to target the patients who need it, so as not to be faced with production problems”, she adds.
“We have to talk about a booster dose, not a third dose”
Regarding the third dose, now required in the future vaccine pass, Claire Andréjak believes that this term is not appropriate. “We should not speak of a third dose but of a booster dose, because after two injections, the vaccination schedule is well finished. The immunity is already there, and the interventions that follow only reboost it”. She also recallsthat rare are the vaccines where a single dose is sufficient. Children are vaccinated against certain diseases (polio, pertussis, tetanus) at 4 months, then have boosters at one year, at 6 years old, sometimes even in adulthood. And to add: “Only the future will tell us if we need to do a second booster dose (or 4 dose, editor’s note), and if so, when will be the right time”.
“Fewer patients in rehearsals with Omicron”
About the Omicron variant, which is making rapid progress throughout France, “the first data show that it is more transmissible but less pathogenic. There will therefore probably be fewer patients in intensive care during this wave, with a rather directed impact on conventional care”, analyzes Claire Andréjak. In the Marseille department of Dr Hervé Pegliasco, “all patients in intensive care are affected by the Delta variant, there are currently no Omicron cases”, confirms the pulmonologist of the European Hospital.
“We will have to get out of tracking, tracing, isolating”
At last, “Sras-cov-2 will not disappear, we will live with it. If Omicron does indeed prove to be very contagious and not very pathogenic, it could replace Delta, allow the long-awaited collective immunity and become a classic winter virus, which we can let it circulate because serious cases will remain limited. Of course, the follow-up is still too weak, and these encouraging trends remain to be confirmed!”, ends Claire Andréjak. And to conclude: “with Omicron, the government strategy of tracking, tracing and isolating will soon no longer be feasible, at some point we will have to get out of it”.
*The antivirals called Molnupiravir (already available) and Paxlovid (under evaluation).
.