A study defines for the first time the disorder of cesarean scar, a lump located in the uterine cavity and accompanied by other symptoms, which affects approximately 25% of women who have given birth by cesarean section.

- A study has just defined C-section scar disorder.
- This is a blister located at the level of the uterine scar.
- This must be accompanied by a primary symptom or two secondary symptoms.
In France, there are approximately 150,000 deliveries performed by caesarean each year and, in 60% of cases, women have a cesarean niche, a phenomenon also called isthmocele. It is a swelling that forms a kind of pocket in the uterine cavity, that is to say the central part of the uterus. This physical manifestation is usually accompanied by other symptoms such as menstrual disorders, pain or infertility.
Cesarean niche: a swelling at the level of the uterine scar
Although caesarean sections have been known to doctors for a long time, there has never been a clear definition of this phenomenon. Thus, 31 international researchers worked to establish the first definition of cesarean scar disorder. Their work has just been published in the journal JAMA Open Network.
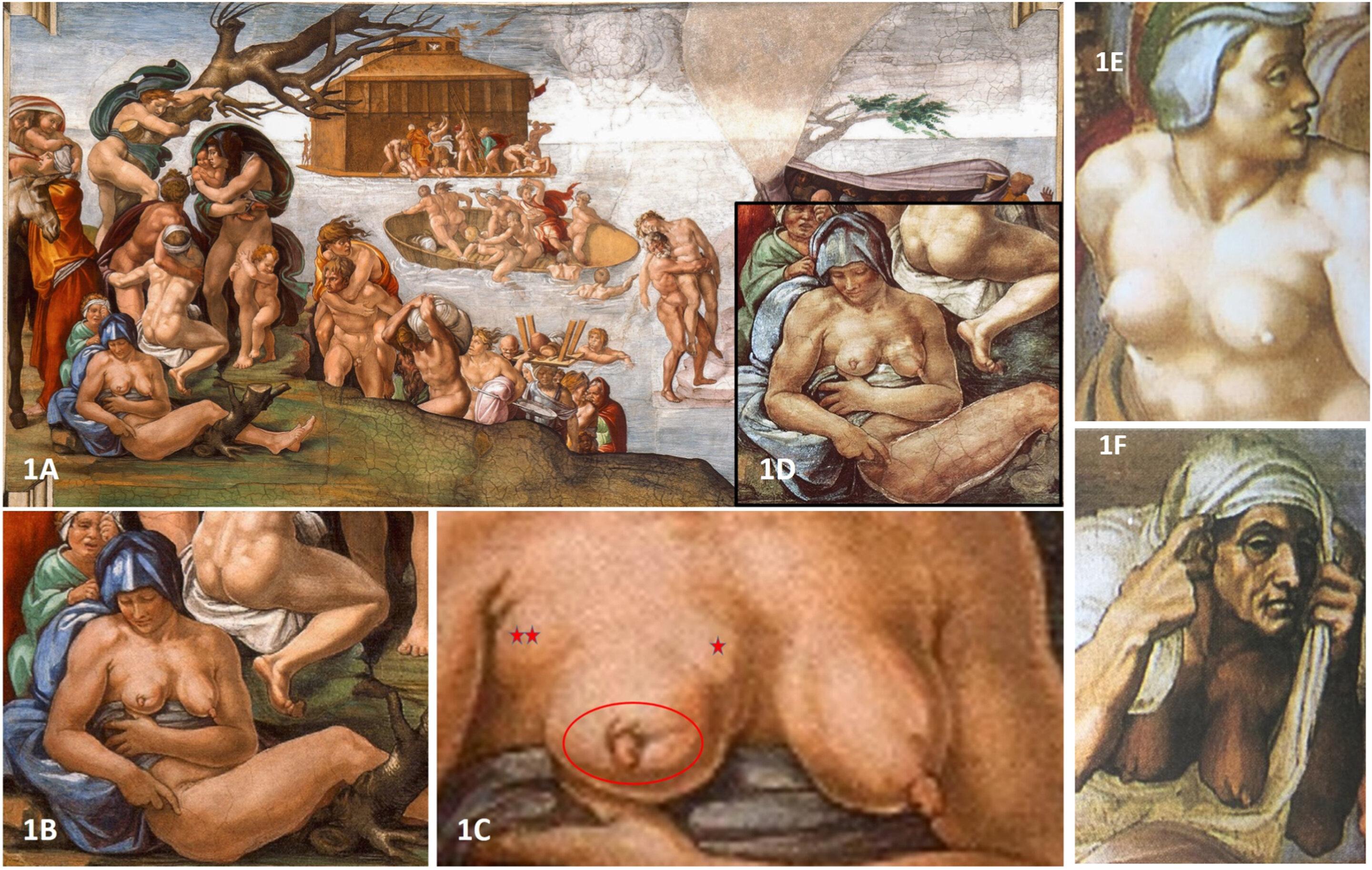
It is therefore a blister located at the level of the uterine scar, which forms a kind of pocket. For scientists, the depression must be at least two millimeters and must be accompanied by at least one so-called “primary” symptom – pain during menstruation, post-menstrual bleeding, unexplained infertility with intrauterine fluids – or else two so-called “secondary” symptoms: pain during intercourse, abnormal vaginal discharge, chronic pelvic pain or abnormal smelly blood loss.
According to the researchers, the diagnosis of cesarean scar disorder can be made if the patient meets these conditions for at least three months after the cesarean section. “Currently the detection and management of cesarean niches is chaotic in France, explains Professor François Goffinet, obstetrician-gynecologist and head of the Maternity Port-Royal department (Paris, AP-HP). Some doctors know and misdetect this problem, and those who do manage it each in their own way.”The idea, with this study, was therefore to allow doctors to better diagnose the disorder of the cesarean scar by defining it in the same way for all practitioners.
Better management of cesarean scar disorder
Until now, cesarean niches were detected during an ultrasound. “The decision to investigate and treat C-section scar disorder is influenced by symptom severity, impact on quality of life, niche size, and individual patient expectations.“, say the experts.
The management of cesarean niches is a surgical intervention. Nevertheless, the method used remains at the discretion of the doctor: electrocoagulation – an electric current destroys the tissues – or remove the affected tissues and then sew them up. “Every day we have patients who are panicked that we have found them a niche for caesarean section, for lack of information, concludes François Goffinet. But when the niche is indeed the source of the symptoms, the intervention is generally effective.”
Once the definition proposed by this new study has been validated by the entire medical profession, the ideal would be to establish a validated standard treatment procedure that all practitioners could follow… And thus reassure the 25% of women affected by a caesarean niche.