Due to the confinement and the closing of borders due to the coronavirus, a Frenchwoman suffering from a rare and aggressive form of brain cancer will not be able to travel to the United States to test a treatment which could have extended her life expectancy by ten years. She told her ordeal to Franceinfo.
-1585759729.jpg)
- A 37-year-old French woman with a brain tumor had to follow a treatment that is only accessible in the United States
- The closing of the borders prevents him from going to the USA
The confinement due to Covid-19 certainly impacts everyone’s life, but the issues are not the same for everyone. Wednesday 1er april on France infoa Frenchwoman living in Denmark and suffering from a brain tumour, tells how the epidemic and the measures taken to try to contain it prevented her from accessing “to the last treatment to slow progression” cancer she has been battling for 16 months.
In November 2018, Célia Curdy-Neves, 37, a lawyer and mother of a three-year-old girl, was diagnosed with Diffuse Midline Glioma (DMG) or diffuse midline glioma. It is a rare and extremely aggressive form of brain tumor. Doctors place his vital prognosis between 18 and 24 months. The patient underwent two operations and several treatments. In vain. The tumor begins to grow again in depth. So much so that it is soon no longer operable. His oncologist then told him about an experimental treatment available at the Presbyterian Hospital in New York (United States) which could extend his life expectancy by ten years. But his tumor, then active, prevents him from following the protocol. Then, a month ago, she learns that she can now claim treatment.
“There I was ready, my suitcase too. After six weeks without any treatment, I could try everything and start the cure on April 6 in the United States”, tells the unfortunate Franceinfo. Unfortunately, on March 11, US President Donald Trump announced a 30-day entry ban on US territory. Three days later, it was Denmark’s turn to close its borders.
Make the most of confinement to create family memories
“We tried to find a ‘political’ derogation to be able to leave Denmark and enter the USA”, she continues. However, a few weeks later, the NY Presbyterian Hospital replies that it must give priority to managing patients with Covid-19. The Danish government offers to make an employee of the Ministry of Health available to her to advance her file, but she refuses. “Even if I manage to get there, the hospital will not accept me, they will not treat me”, explains Celia.
Why couldn’t the patient receive her treatment by post? The pharmaceutical company Oncoceutics, which produces the ONC21 treatment it needs, originally planned to expand into Europe in late 2019.”But in February, they changed their minds laments Celia. Few patients suffer from this pathology so there is little money to be made”, she says, indignant. How, ethically, can the laboratory refuse access to treatment? For me, it’s non-assistance to anyone in danger! How am I going to explain to my 3-year-old daughter that she won’t be having her mom soon because people refuse to put pills in a cardboard box and send them to me?.”
Every day, Célia goes to the White House site to see when flights between Europe and the United States will resume, while being aware that once the borders are open, the United States will have to control the Covid-19 health crisis completely. However, New York is one of the cities hardest hit by the pandemic.
If on the Danish side, the borders are supposed to reopen on April 14, “everyone thinks it’s going to be extended”, declares Célia who tries to make the most of her daughter while waiting. “We create lots of memories, it’s the positive side of confinement all these moments together that she will keep for later. Same with her husband. My husband and I know we will not grow old together. So I try to put aside this cancer as much as possible to live the little pleasures of life”, she testifies.
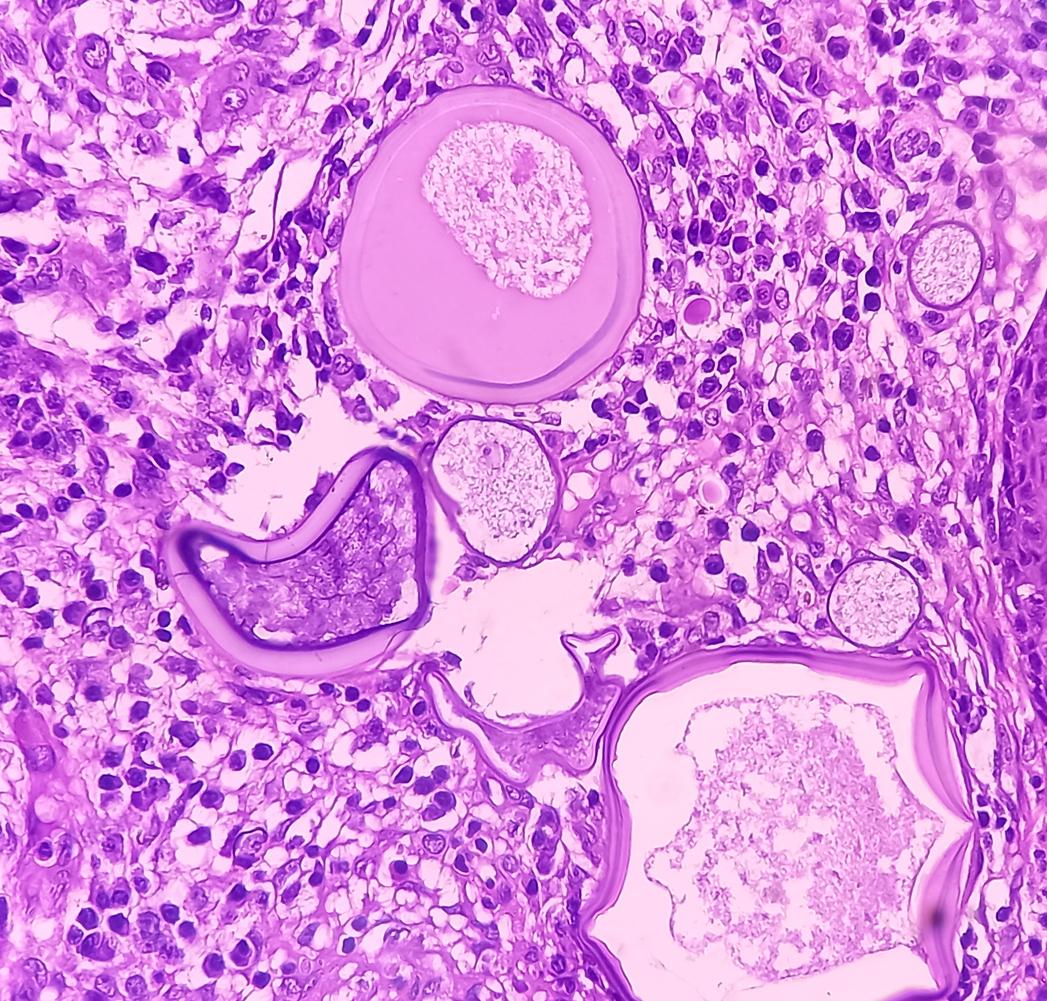
What is diffuse midline glioma?
Diffuse midline glioma is a rare, aggressive and rapidly growing subtype of glial tumors. Diffuse midline glioma most commonly forms in the pons of the brainstem, thalamus, spinal cord, and cerebellum. Because diffuse midline gliomas grow rapidly, they can spread to other areas of the central nervous system (CNS) through the cerebrospinal fluid. The tumor can then invade nearby tissues and extend beyond what can be seen on MRI or by the surgeon during the operation.
Because, if possible, the first treatment for diffuse midline gliomas is surgery. The goal is to determine the type of tumor and remove as many as possible without causing side effects. Since the brainstem, thalamus and spinal cord are sensitive areas of the CNS, operating in these areas can lead to severe loss of function. But if the risk of a biopsy is deemed too high, diffuse midline glioma can sometimes be treated with radiation therapy alone. Usually, in addition to surgery, the disease requires additional treatments such as radiation therapy, chemotherapy, or clinical trials. Targeted therapy or immunotherapy can also be considered, depending on each patient.
In terms of symptoms, patients may suffer from vision problems, swallowing, weakness and loss of balance. The tumor can also cause increased pressure inside the skull due to excessive production of cerebrospinal fluid or blockage of normal flow. This is called hydrocephalus. The latter can be characterized by nausea, vomiting, irritability, headaches, blurred or double vision, a strong desire to sleep and seizures. People with a diffuse midline spinal glioma may also experience progressive weakness, numbness, and problems with bowel and bladder control.

.