For the first time, a team of researchers has managed to 3D print human skin, blood vessels included. A spectacular advance that gives hope for future skin grafts fully integrated into the patient’s skin.

This is a landmark first in the field of 3D bioprinting.
In an article published in the journal Tissue Engineering Part A, scientists from Rensselaer Polytechnic Institute in the United States, explain that they have developed a way to 3D print living and vascularized human skin. A great first which is an important step towards the creation of grafts that look more like the skin that our body produces naturally.
A “bio-ink” that grafts onto human skin
Until now, attempts to achieve using 3D bioprinting of human tissues have come up against a difficulty: that of the absence of a functional vascular system in the grafts.
“Right now, anything available as a clinical product is more like a fancy bandage,” said Pankaj Karande, who led the work. “It speeds up healing, but eventually it falls off, it never really integrates with the host cells.”
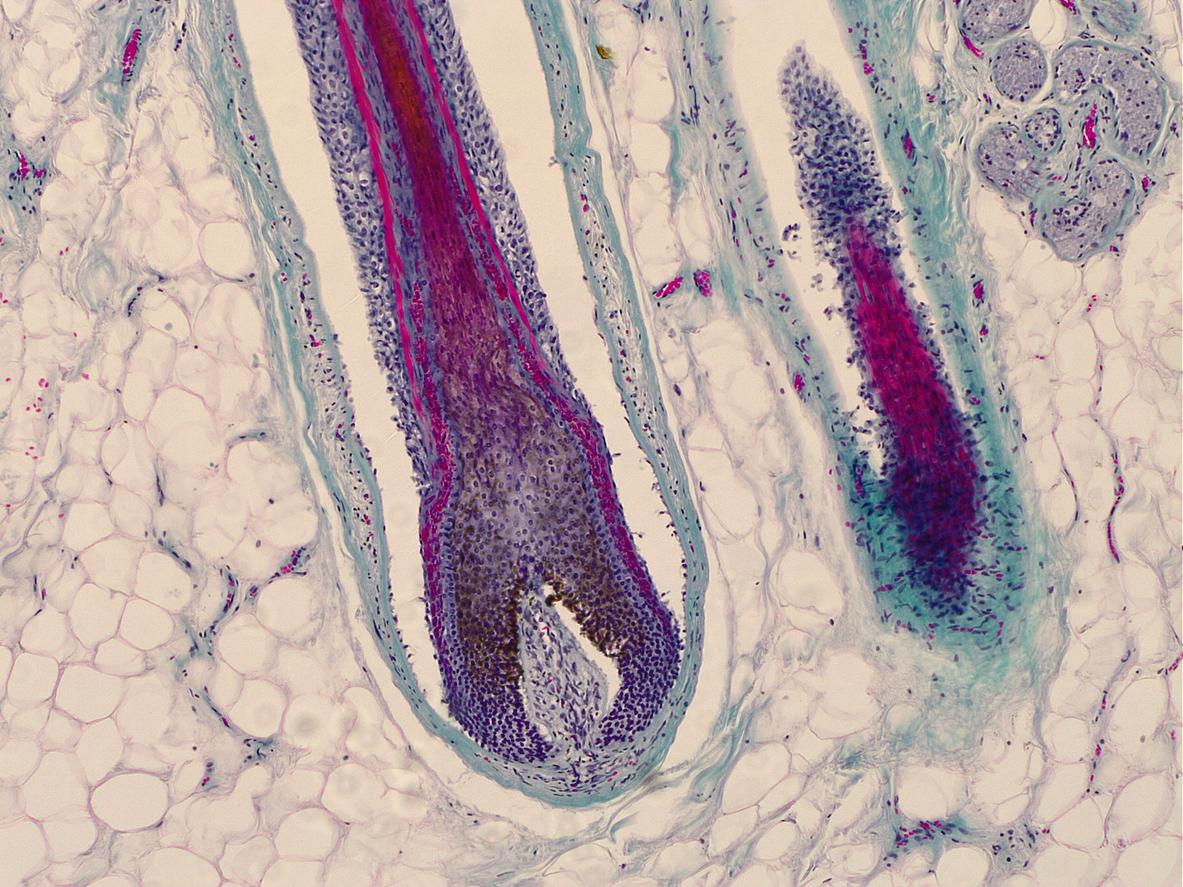
The challenge faced by the researchers was therefore to recreate this vascularization in the 3D printed grafts. Professor Karande has worked on the subject for many years and shown in previous work that it is possible to take two types of human cells and transform them into “bio-inks” in order to imprint them in a structure similar to skin. .
This new research goes further because the researchers have added to this “bio-ink” human endothelial cells, which line the interior of blood vessels, and human periclite cells, which surround the endothelial cells. Thus, the cells began to communicate with each other and form a vascular structure in just a few weeks.
No clinical trial in sight yet
Once the graft was made, the scientists grafted it onto a mouse. They then found that the imprinted blood vessels began to communicate and connect with those of the rodent. “This is extremely important, because we know that there is actually a transfer of blood and nutrients to the graft, which keeps the graft alive,” explains Professor Karande.
Many steps are still necessary before making this technology usable at the clinical level. In particular, researchers must succeed in editing donor cells using CRISPR technology so that the vessels can integrate and be accepted by the patient’s body. “We’re still not there, but we’re a bit closer today,” said the lead researcher.
If the objective of the authors of the study is to produce grafts for severe burn victims with loss of nerve and vascular endings, the path will be long. For the moment, the grafts created could mainly help patients suffering from diabetes or pressure sores. “For these patients, it would be perfect, because ulcers usually appear in different places on the body and can be treated with smaller pieces of skin,” argues Professor Karande. “Healing generally takes longer in diabetic patients, and this could also help speed up the process.”
.