In the long term, the bacteria that cause gum disease would cause inflammation and degeneration of brain neurons similar to those of Alzheimer’s disease.

Can periodontal disease cause neurological degeneration comparable to that of Alzheimer’s disease? This is the thesis defended by researchers at the University of Illinois, in the United States. In an article published Wednesday, October 3 in the journal PLOS One, they explain having studied the effects of periodontal bacteria on the development of neurodegenerative diseases such as Alzheimer’s.
“Other studies have shown a strong association between periodontitis and cognitive impairment, but this is the first study to show that exposure to periodontal bacteria results in the formation of senile plaques which accelerate the development of neuropathology in patients with the disease. Alzheimer’s disease, “said Dr. Keiko Watanabe, UIC faculty of dentistry professor of periodontics and lead author of the study, in a statement.
Migration of the bacteria to the brain
Periodontal disease (or periodontitis) is an infectious disease that affects and destroys the supporting tissues of the teeth. It is generally a slow disease, which evolves over several decades and is caused by the stagnation of bacteria in the dental plaque, which creates an inflammatory reaction on the gums and bones. If it can be slowed down on a daily basis thanks to careful dental and oral hygiene, periodontitis unfortunately cannot be cured.
In order to study the link between periodontal bacteria and neurodegenerative diseases, Dr. Wanatabe’s team established chronic periodontitis in 10 mice characterized by soft tissue damage and bone loss in the oral cavity. Another 10 mice served as a control group.
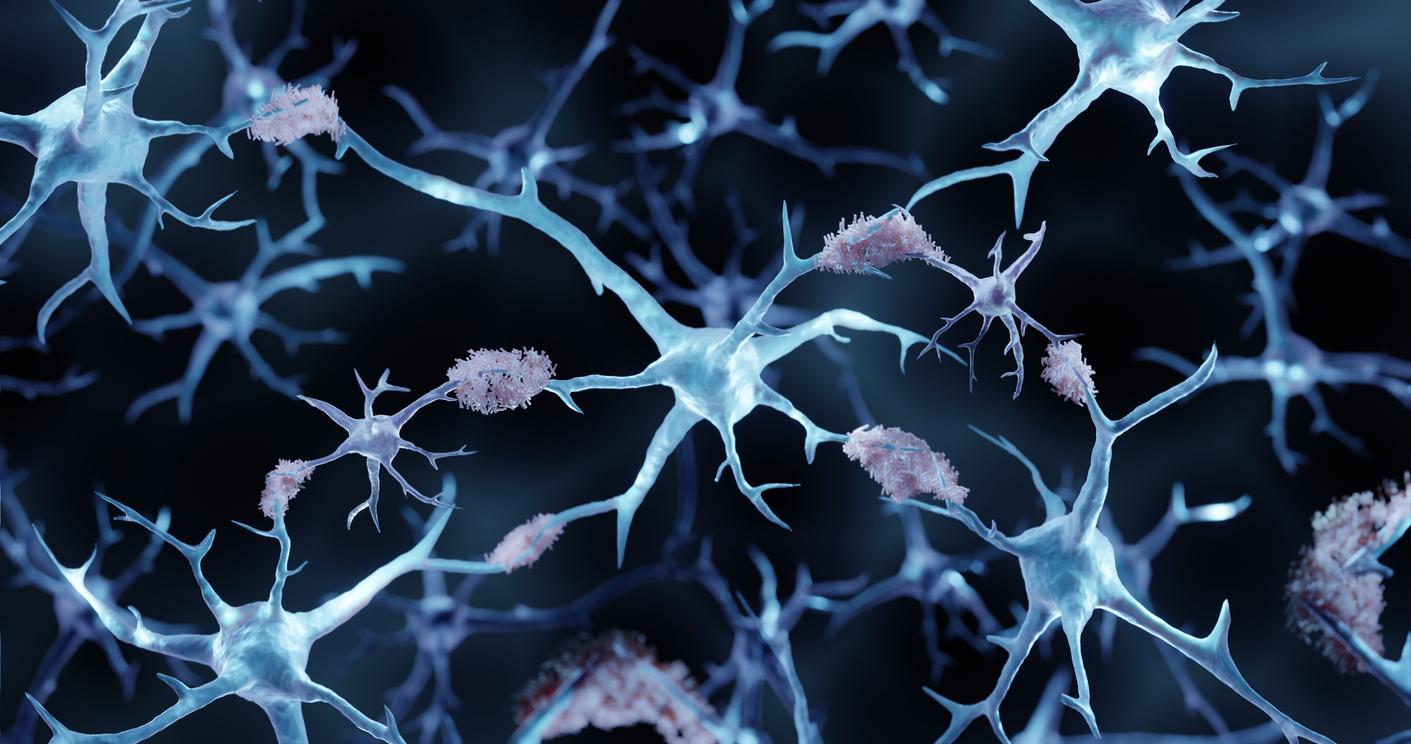
After 22 weeks of repeated oral application of the bacteria, the researchers studied the brain tissue of the mice and compared their health. Mice chronically exposed to the bacteria were found to have significantly higher amounts of accumulated beta-amyloid protein. Their brains were also more inflamed and had fewer intact neurons due to degeneration.
These results were also corroborated by beta-amyloid protein analysis and RNA analysis which showed greater expression of genes associated with inflammation and degeneration in the study group. In addition, traces of the periodontal bacteria were also found in the brain tissue of mice, and a bacterial protein was observed inside their neurons. “Our data demonstrate not only the movement of bacteria from the mouth to the brain, but also that chronic infection leads to neural effects similar to those of Alzheimer’s disease,” says Dr Wanatabe.
Oral hygiene as a predictor of disease
For the researchers, these results are all the more convincing since the mice used were not rodents genetically modified to express more strongly the genes of Alzheimer’s disease, but wild mice. “These mice were not prepared for the development of the disease, and the use of this model gives additional weight to our conclusions that a periodontal bacterium could restart the development of Alzheimer’s disease,” says the researcher.
For Dr Wanatabe, the results of this new work clearly show that understanding the causality and risk factors for the development of Alzheimer’s disease is essential for developing new treatments. This is all the more true with degenerative diseases which develop late and whose mechanisms are still largely unknown.
Oral health is one of them. For Dr Wanatabe, such results must be measured by all. “Oral hygiene is a strong predictor of disease, including diseases that occur outside the mouth. People can do a lot for their personal health by taking oral health seriously,” she said. declared.


.