Myelodysplastic syndromes are thought to be linked to a dysfunction of a gene involved in the metabolism and oxygenation of blood cells. This makes the HIF1A gene a potential therapeutic target.
A team of scientists from the Cincinnati Children’s Hospital Center may be solving the mystery surrounding the origins of a group of complex, heterogeneous blood diseases that are currently incurable and can lead to leukemias. Myelodysplastic syndromes are associated with a number of genetic mutations and are considered to be one of the most complex blood diseases. It is also a pre-cancerous situation.
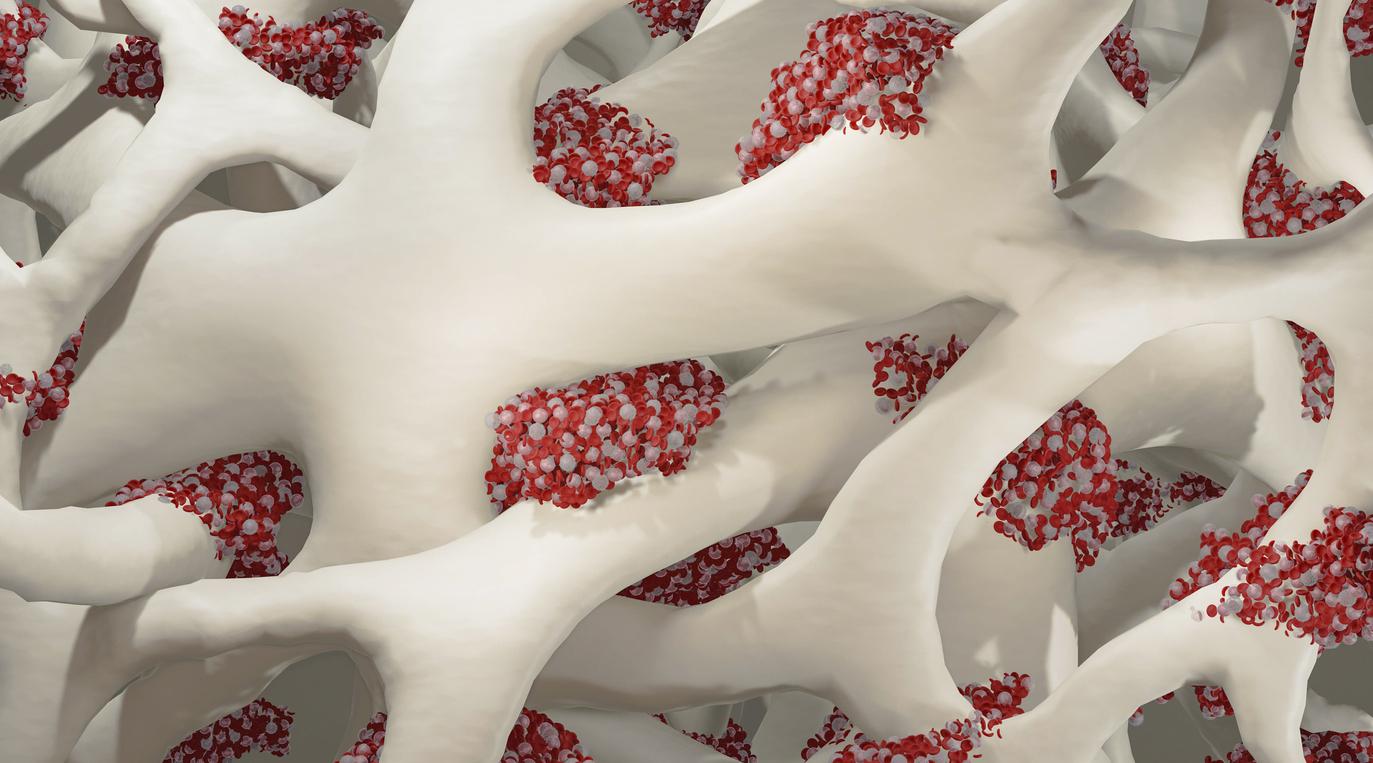
Myelodysplastic syndromes affect the hematopoietic stem cells in the bone marrow. According to Gang Huang, principal investigator of this new study, a new gene has been identified in these cells which would be able to trigger the various biological processes at the origin of the various types of myelodysplastic syndromes observed in patients.
The mechanism in question is thought to be that of a paradoxical activation in the bone marrow of the HIF1A gene, a gene involved in the metabolism and oxygenation of precursor cells of blood cells. The results are published in the journal Cancer Discovery.
Myelodysplastic syndromes suffocate the bone marrow
Called myelodysplastic syndromes (MDS), these syndromes are responsible for the appearance of immature cells in the bone marrow, which becomes dysfunctional with insufficient production of healthy mature cells.
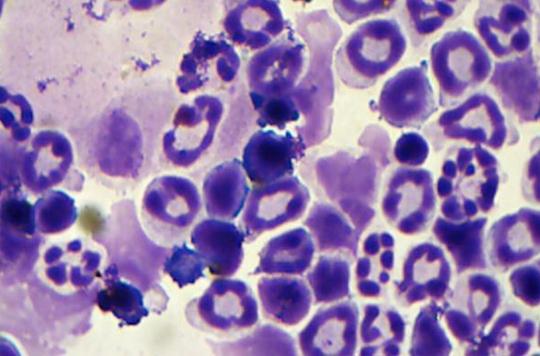
Immature blood cells, called blasts, do not work properly. They accumulate in the bone marrow and in the blood, where there are therefore fewer healthy red blood cells (anemia), white blood cells (leukopenia) and platelets (thrombocytopenia). The main risk is that of a progression to leukemia.
No curative treatment for most patients
The only current treatments are essentially aimed at compensating for the deleterious effects of insufficient production of healthy blood cells. A few molecules directed against abnormalities observed during myelodysplastic syndromes are in the testing phase. But the only real curative treatment today is a bone marrow transplant.
Unfortunately, the frequency of myelodysplastic syndromes increases with aging and the median age of patients is around 70 years. Thus, a bone marrow transplant is only possible in a very limited number of cases, in particular because the oldest people suffering from this disease are not healthy enough to tolerate a hematopoietic stem cell transplant.
A regulatory gene for metabolism and oxygen
“We know that the genomes of patients with myelodysplastic syndromes have recurrent mutations in different transcriptional, epigenetic and metabolic regulators, but the incidence of these mutations does not directly correlate with the disease when it appears.” “Our study shows that dysfunctional activation of the HIF1A gene could cause the various medical problems that physicians see in patients with myelodysplastic syndromes.”
The HIF1A (hypoxia inducible factor 1) gene is a transcription factor, a regulatory gene that tells other genes what to do. HIF1A therefore plays an essential role in the response of cells to changes in metabolism and oxygen levels. As a result, it affects the functioning of more than a thousand genes. This includes a vital role in regulating the biological functions of blood cell-producing hematopoietic stem cells in the bone marrow.
The central role of the HIF1A regulatory gene
Huang and his colleagues first found the consistent implication of the HIF1A gene dysfunction by studying cells from patients with myelodysplastic syndrome through in-depth analyzes.
They then demonstrated in different animal models that deregulation of the HIF1A gene played a central role in the appearance of different types of myelodysplastic syndromes, their complications and their symptoms.
Finally, by experimentally eliminating the HIF1A signaling in a mouse model of myelodysplastic syndrome, the researchers have shown that inhibition of the HIF1A gene eliminates a number of symptoms usually observed.
Possible therapeutic target
Although the researchers insist that more research is needed before whether their results will become clinically useful, their study indicates that the HIF1A gene is a potential therapeutic target for a disease where treatments are primarily palliative.
The main problem is that most of the HIF1A inhibitors available today also target a second related molecule, called HIF2A. This is what prevents the use of these inhibitors in patients suffering from a myelodysplastic syndrome.
.